Postpartum Care
Postpartum Care
The postpartum period, also known as the puerperium, encompasses the six weeks following childbirth during which a woman’s body undergoes significant physiological changes as it returns to a pre-pregnancy state. This chapter on Postpartum Care delves deeply into the physical recovery aspects of the postpartum period, focusing on the involution of the uterus, perineal care, and breast care. Each of these components is crucial for ensuring a smooth recovery and promoting overall maternal well-being.
Physical Recovery
Physical recovery in the postpartum period is critical for the new mother’s health and well-being. It involves several key aspects, including the involution of the uterus, perineal care, and breast care. Each of these areas requires thorough monitoring and appropriate interventions to address potential complications and support recovery.
Involution of the Uterus
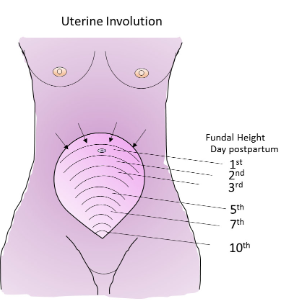
Involution refers to the process by which the uterus returns to its pre-pregnancy size and condition following childbirth. This process typically begins immediately after delivery and continues for several weeks.
Monitoring Uterine Firmness and Location:
i. Assessment Techniques:
- Fundal Height Measurement: The fundus, or the top of the uterus, should be palpated regularly to monitor its descent. Postpartum, it is initially located at or near the umbilicus. By the second day, it typically descends to about 1-2 cm below the umbilicus, and by 10-14 days, it should be within the pelvis.
- Uterine Tone: The firmness of the uterus is assessed by palpation. A firm uterus indicates proper involution and contraction, while a boggy or soft uterus may suggest uterine atony, which requires intervention.
ii. Uterine Atony Management:
- Pharmacological Interventions: Medications such as oxytocin (Pitocin) are administered to stimulate uterine contractions and reduce the risk of hemorrhage.
- Manual Uterine Compression: If the uterus is found to be boggy despite medication, manual compression or massage may be performed to encourage contraction.
iii. Ultrasound Examination:
- Assessment of Uterine Size and Position: In cases of suspected complications, such as retained placental fragments or abnormal bleeding, ultrasound may be used to evaluate the uterine size and detect any abnormalities.
Managing Lochia (Postpartum Bleeding):

i. Understanding Lochia:
- Types of Lochia: Lochia is the vaginal discharge after childbirth, which progresses through three stages: lochia rubra (red), lochia serosa (pink to brown), and lochia alba (white to yellow). This discharge consists of blood, mucus, and uterine tissue.
- Normal Duration and Amount: Lochia rubra lasts for about 3-4 days, lochia serosa for an additional 4-10 days, and lochia alba for up to 4-6 weeks.
ii. Monitoring and Management:
- Assessment of Volume and Characteristics: The amount, color, and odor of lochia are assessed. Excessive bleeding (saturation of more than one peri pad per hour) or foul odor may indicate complications such as postpartum hemorrhage or infection.
- Patient Education: Mothers should be educated on what constitutes normal versus abnormal lochia. They should be advised to use maternity pads rather than tampons to prevent infection and to report any concerns immediately.
iii. Complications:
-
- Postpartum Hemorrhage (PPH): Defined as blood loss exceeding 500 mL after vaginal delivery or 1000 mL after cesarean section. Early identification and intervention are crucial. Common causes include uterine atony, retained placental fragments, and lacerations.
- Management Strategies: PPH management includes uterine massage, medications (e.g., oxytocin, methylergometrine), and, if necessary, surgical interventions.
Perineal Care
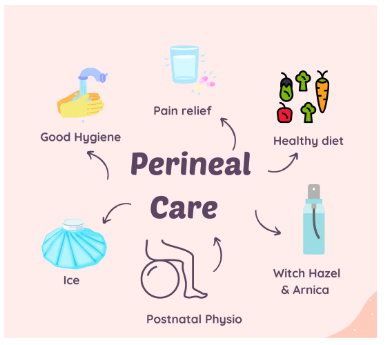
Perineal care involves managing the area between the vaginal opening and the anus, which can be affected by childbirth. This care is vital for preventing infection and promoting healing.
Healing and Care of Episiotomy or Lacerations:
Types of Perineal Trauma:
- Episiotomy:
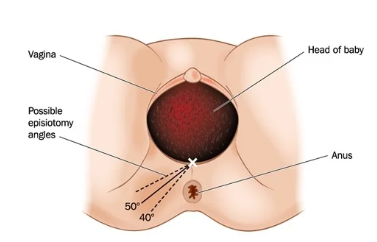
A surgical incision made in the perineum during delivery to enlarge the vaginal opening. It may be midline or mediolateral.
- Lacerations:
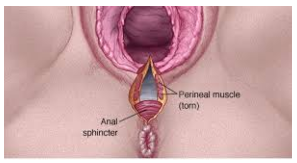
Natural tears that occur during childbirth, classified into four degrees based on severity (first-degree superficial, second-degree involving muscle, third-degree involving the anal sphincter, and fourth-degree involving the rectal mucosa).
i. Assessment and Care:
- Inspection: Regular inspection of the perineal area for signs of infection, excessive bleeding, or delayed healing. This includes checking for redness, swelling, or discharge.
- Pain Management: Pain relief can be managed with analgesics (e.g., acetaminophen, ibuprofen), topical anesthetics, and ice packs. Sitz baths can also provide comfort and aid in healing.
- Hygiene Practices: Keeping the perineal area clean and dry is essential. Mothers should be instructed to use peri bottles to cleanse the area after each void or bowel movement and to avoid douching or using harsh soaps.
ii. Complications:
- Infection: Signs include increased pain, fever, and purulent discharge. Prompt treatment with antibiotics is essential.
- Dehiscence or Evisceration: Rare but serious complications where the episiotomy or laceration site may open or fail to heal properly. Surgical intervention may be required.
Breast Care

Breast care is crucial for managing lactation and addressing common issues that arise during breastfeeding. Proper care supports successful breastfeeding and maternal comfort.
Managing Lactation and Breastfeeding Support:
i. Breastfeeding Initiation:
- Latching Techniques: Proper latching is critical for effective breastfeeding and preventing nipple pain. The infant’s mouth should cover the areola, not just the nipple.
- Feeding Frequency: Newborns typically feed every 2-3 hours. Monitoring the frequency and duration of feedings helps ensure adequate milk intake.
ii. Milk Production:
- Breast Milk Composition: Colostrum, the first milk, is rich in antibodies and nutrients. Transitional milk follows, and mature milk is produced by around 2 weeks postpartum.
- Increasing Milk Supply: Techniques to enhance milk production include frequent breastfeeding, proper hydration, and use of lactation aids if needed.
iii. Breastfeeding Challenges:
- Nipple Pain and Cracks: Often caused by improper latching or friction. Using nipple creams, ensuring proper latch, and allowing nipples to air dry can alleviate discomfort.
- Engorgement: Caused by an overproduction of milk or infrequent feeding. Symptoms include swollen, tender breasts. Solutions include frequent breastfeeding, warm compresses, and milk expression.
Addressing Common Issues:
i. Mastitis:
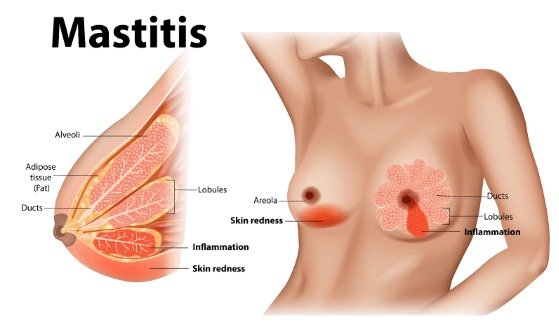
- Definition and Symptoms: An infection of the breast tissue characterized by redness, swelling, pain, and fever. It typically results from a blocked milk duct or bacterial infection.
- Management: Treatment includes antibiotics, frequent breastfeeding or milk expression, and applying warm compresses. Ensuring complete emptying of the breast helps prevent recurrence.
ii. Blocked Milk Ducts:
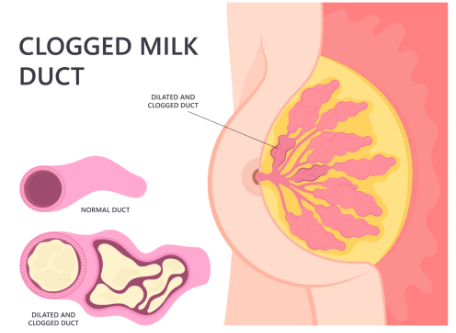
- Identification and Care: Symptoms include a tender lump in the breast. Treatment involves frequent breastfeeding, massage of the affected area, and warm compresses.
iii. Breast Abscess:
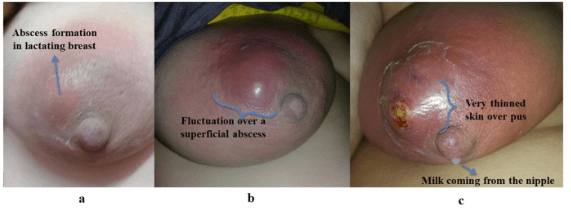
- Signs and Treatment: A localized collection of pus in the breast tissue. Treatment may involve incision and drainage, along with antibiotics. Supportive measures include breastfeeding from the unaffected breast and using a breast pump.
Conclusion
Comprehensive postpartum care is essential for the physical recovery of the mother following childbirth. It involves careful monitoring of uterine involution, effective management of perineal trauma, and thorough support for breastfeeding. Addressing these aspects with detailed assessment and timely interventions can significantly enhance maternal recovery, reduce complications, and support overall well-being. Each component—uterine involution, perineal care, and breast care—plays a vital role in ensuring a smooth transition into the postpartum period and promoting long-term health for the new mother.
Psychological and Emotional Support
The postpartum period not only involves physical recovery but also significant psychological and emotional adjustments. This chapter on Postpartum Care explores the critical aspects of Psychological and Emotional Support, focusing on Postpartum Depression and Adjustment to Parenthood. These areas are essential for ensuring the well-being of new mothers and their infants.
Psychological and Emotional Support

Psychological and emotional support during the postpartum period is crucial for a mother’s overall recovery and adjustment to new motherhood. This support encompasses recognizing and addressing postpartum depression and facilitating a smooth transition into parenthood.
Postpartum Depression

Postpartum Depression (PPD) is a serious mental health condition affecting many new mothers. It is more than just the “baby blues” and can significantly impact a woman’s ability to care for herself and her baby.
Screening and Identifying Risk Factors:
i. Screening Methods:
- Edinburgh Postnatal Depression Scale (EPDS): A widely used tool consisting of 10 questions that assess symptoms of depression in the postpartum period. A score of 10 or more suggests a higher likelihood of postpartum depression.
- Patient Health Questionnaire-9 (PHQ-9): An assessment tool used to evaluate the severity of depressive symptoms. It is applicable for diagnosing depression in various stages, including postpartum.
ii. Risk Factors:
- Previous Mental Health Issues: Women with a history of depression or anxiety are at higher risk for developing PPD.
- Lack of Support: Social isolation or lack of support from family and friends can increase the risk.
- Complications During Pregnancy or Delivery: Traumatic birth experiences, preterm delivery, or neonatal complications can contribute to PPD.
- Unplanned Pregnancy: Unplanned or unwanted pregnancies can be associated with higher levels of stress and anxiety.
- Hormonal Changes: The rapid hormonal fluctuations after childbirth can affect mood and contribute to depressive symptoms.
iii. Signs and Symptoms:
- Emotional Symptoms: Persistent feelings of sadness, hopelessness, or emptiness; extreme mood swings.
- Behavioral Symptoms: Withdrawal from family and friends, loss of interest in activities once enjoyed.
- Cognitive Symptoms: Difficulty concentrating, making decisions, or remembering things.
- Physical Symptoms: Changes in sleep patterns, appetite disturbances, and fatigue.
Referral to Mental Health Services:
i. Identifying Need for Referral:
- Severity of Symptoms: Persistent or severe symptoms of depression that interfere with daily functioning require professional intervention.
- Risk of Self-Harm or Harm to Others: Immediate referral is necessary if there are any signs of self-harm, suicidal ideation, or harm to the baby.
ii. Types of Mental Health Services:
- Psychiatric Evaluation: Comprehensive assessment by a psychiatrist to diagnose and determine the appropriate treatment plan.
- Therapy Options: Cognitive-behavioral therapy (CBT), interpersonal therapy (IPT), or other evidence-based therapies can help address depressive symptoms.
- Medication: Antidepressants may be prescribed if necessary. It is essential to discuss the risks and benefits of medication with the healthcare provider, particularly regarding breastfeeding.
iii. Support Services:
- Support Groups: Peer support groups for postpartum women can provide emotional support and reduce feelings of isolation.
- Counseling Services: Individual or family counseling can help address relational issues and enhance coping strategies.
Adjustment to Parenthood
Adjustment to Parenthood involves adapting to the new roles and responsibilities that come with being a parent. This adjustment is critical for the well-being of both the mother and the infant and involves fostering maternal-infant bonding and providing education on infant care.
Supporting Maternal-Infant Bonding:

i. Understanding Bonding:
- Definition: Maternal-infant bonding refers to the emotional connection that develops between a mother and her baby. This bond is crucial for the baby’s emotional and physical development.
- Importance: Strong bonding is associated with better attachment, emotional security, and overall health of the infant.
ii. Facilitating Bonding:
- Skin-to-Skin Contact: Immediate and continuous skin-to-skin contact after birth helps promote bonding, regulate the baby’s temperature, and stabilize the baby’s heart rate and breathing.
- Responsive Parenting: Responding promptly to the baby’s cues (crying, feeding, comfort) fosters a secure attachment and builds trust.
- Breastfeeding Support: Breastfeeding not only provides nutritional benefits but also enhances bonding through physical closeness and eye contact.
iii. Challenges to Bonding:
- Postpartum Depression: Depression can hinder the bonding process. Addressing PPD and seeking appropriate treatment can help improve maternal-infant interactions.
- Premature or Ill Infants: Babies born prematurely or with health issues may require special care, which can affect bonding. Providing support and facilitating bonding activities, even in the NICU, is important.
Providing Education on Infant Care:
i. Basic Infant Care:
- Feeding:

Education on breastfeeding techniques, formula feeding, and recognizing hunger cues is essential. Instructions on feeding frequency, burping, and introducing solids at the appropriate time are also important.
- Diapering and Hygiene:

Proper diapering techniques, maintaining hygiene, and recognizing signs of diaper rash are key areas of education. Instructions on cord care and bath time should also be provided.
- Sleep Patterns:
Information on safe sleep practices, establishing sleep routines, and recognizing normal sleep patterns helps prevent sudden infant death syndrome (SIDS) and promotes healthy sleep habits.
ii. Infant Development:
- Developmental Milestones: Educating parents about typical developmental milestones (e.g., rolling over, sitting up, crawling) helps set realistic expectations and identify any concerns early.
- Stimulating Development: Guidance on activities that promote cognitive and motor development, such as tummy time and interactive play, supports the baby’s growth.
iii. Emergency Care:
- Recognizing Illness:

Training on recognizing signs of common infant illnesses, such as fever, colic, or respiratory issues, and when to seek medical attention.
- Basic First Aid: Providing basic first aid training for emergencies, such as choking, fever management, and CPR, enhances parents’ confidence and preparedness.
Conclusion
Comprehensive postpartum care includes not only physical recovery but also significant psychological and emotional support. Addressing Postpartum Depression through effective screening, identifying risk factors, and referring to mental health services is essential for maternal well-being. Supporting Adjustment to Parenthood involves fostering maternal-infant bonding and providing education on infant care. By addressing these aspects, healthcare providers can support new mothers in their transition to parenthood, promoting overall health and well-being for both mother and baby.
Patient Education and Discharge Planning
Effective patient education and discharge planning are integral to postpartum care. They help new mothers manage their recovery, navigate the challenges of early motherhood, and access necessary follow-up care. This section provides extensive coverage of Self-Care strategies and the importance of Follow-Up Appointments.
Self-Care
Self-care is essential for postpartum recovery and overall health. It involves managing physical well-being through activity and exercise, proper nutrition, and adequate hydration.
Activity and Exercise Guidelines:
i. Importance of Activity:
- Physical Recovery: Gentle physical activity helps with the recovery of muscle tone, improves circulation, and reduces the risk of postpartum complications such as deep vein thrombosis (DVT) and constipation.
- Mental Well-being: Exercise can help alleviate symptoms of postpartum depression, reduce stress, and improve overall mood by releasing endorphins.
ii. Postpartum Activity Recommendations:
- Initial Rest:

Immediately postpartum, it is essential to rest and allow the body to recover from childbirth. Avoid strenuous activities and heavy lifting for the first few weeks.
- Gradual Increase: Begin with light activities such as walking and gradually increase intensity based on comfort and energy levels. Aim for short, frequent walks to start.
- Pelvic Floor Exercises:

Kegel exercises can help strengthen the pelvic floor muscles, which may be weakened during pregnancy and childbirth. Regular practice can improve bladder control and reduce the risk of pelvic organ prolapse.
- Abdominal Exercises:
After receiving medical clearance, engage in gentle abdominal exercises to strengthen core muscles. Avoid high-impact exercises until the body has fully healed.
iii. Guidance for Exercise:
- Listen to Your Body: Postpartum women should be encouraged to listen to their bodies and avoid pushing through pain or discomfort. Any new or worsening symptoms should be discussed with a healthcare provider.
- Hydration and Nutrition: Adequate hydration and nutrition support exercise and overall recovery. Drinking plenty of fluids and maintaining a balanced diet enhances energy levels and promotes healing.
Nutrition and Hydration:
i. Nutritional Needs:

Balanced Diet: A well-balanced diet is crucial for postpartum recovery. Emphasize the importance of consuming a variety of foods rich in vitamins, minerals, and proteins to support healing and energy levels.
Increased Caloric Needs: Breastfeeding mothers may require additional calories to support milk production. Aiming for a nutrient-dense diet helps meet both caloric and nutritional needs.
Key Nutrients:
- Iron: Essential for replenishing blood loss from childbirth and combating postpartum fatigue. Sources include lean meats, beans, and fortified cereals.
- Calcium and Vitamin D: Important for bone health, especially for breastfeeding mothers. Include dairy products, leafy greens, and fortified foods.
- Fiber: Helps prevent constipation, which is common postpartum. High-fiber foods include fruits, vegetables, whole grains, and legumes.
ii. Hydration:

- Importance of Hydration: Adequate fluid intake is essential for maintaining milk production, supporting overall health, and preventing dehydration.
- Recommended Intake: Aim for at least 8-10 glasses of water per day, adjusting based on individual needs and activity levels. Herbal teas and broths can also contribute to hydration.
iii. Practical Tips:
- Meal Planning: Encourage meal planning and preparation before delivery to ensure access to healthy foods. Preparing and freezing meals in advance can ease the transition to new routines.
- Healthy Snacking: Stocking up on healthy snacks such as nuts, fruits, and yogurt can provide quick energy and support nutritional needs during busy postpartum days.
Follow-Up Appointments
Follow-up appointments are crucial for monitoring postpartum recovery, addressing any complications, and providing ongoing support to new mothers. These visits are integral to ensuring comprehensive care and promoting long-term health.
Scheduling and Importance of Postpartum Visits:
i. Timing of Follow-Up Appointments:

- First Postpartum Visit: Typically scheduled within 1-2 weeks after childbirth. This visit allows for the assessment of physical recovery, evaluation of any complications, and discussion of postpartum concerns.
- Subsequent Visits: Additional follow-up appointments may be scheduled at 6 weeks postpartum to assess overall recovery, address ongoing issues, and provide preventive care.
ii. Components of Postpartum Visits:
- Physical Examination: Assessment of uterine involution, perineal healing, and overall physical recovery. Monitoring vital signs, weight, and any signs of complications such as infection or hemorrhage.
- Mental Health Screening: Evaluation of psychological well-being, including screening for postpartum depression or anxiety. Providing referrals to mental health professionals if needed.
- Breastfeeding Support: Addressing any issues related to breastfeeding, such as latch problems, pain, or milk supply concerns. Offering guidance and support for successful breastfeeding.
- Contraceptive Counseling: Discussing and selecting appropriate contraceptive methods based on individual preferences and health considerations.
iii. Importance of Follow-Up Care:
- Monitoring Recovery: Regular follow-up helps ensure that any complications are identified and managed early. It allows healthcare providers to track progress and provide necessary interventions.
- Addressing Concerns: Follow-up visits offer an opportunity for new mothers to ask questions, voice concerns, and receive education on postpartum care, infant care, and family planning.
- Promoting Well-being: Ongoing care supports mental and physical health, promotes effective breastfeeding, and helps new mothers transition to parenthood more smoothly.
iv. Patient Education on Follow-Up:
- Understanding the Purpose: Educate patients on the importance of attending follow-up appointments and what to expect during these visits. Emphasize that these visits are a routine part of postpartum care aimed at ensuring health and well-being.
- Preparing for Appointments: Encourage patients to prepare a list of questions or concerns to discuss during follow-up visits. Keeping track of any symptoms or issues that arise can facilitate more effective consultations.
Conclusion
Comprehensive Patient Education and Discharge Planning are fundamental components of postpartum care. Self-Care encompasses activity and exercise guidelines, nutrition, and hydration, all crucial for promoting recovery and well-being. Follow-Up Appointments ensure ongoing monitoring and support, addressing any complications and providing essential care. By focusing on these aspects, healthcare providers can support new mothers in their postpartum journey, enhancing their overall health and facilitating a successful transition to parenthood.
