N: Nutritional Needs Across the Lifespan
Nutritional Needs Across the Lifespan: Infants and Children
-
Infants and Children

Nutritional Requirements
Breastfeeding and Formula Feeding
Benefits of Breastfeeding: Breastfeeding is recommended as the exclusive source of nutrition for infants for the first six months of life. It provides numerous health benefits, including:
- Optimal Nutrition: Breast milk is tailored to an infant’s nutritional needs, providing the right balance of proteins, fats, and carbohydrates, as well as vitamins and minerals.
- Immune Protection: Breast milk contains antibodies and other immunological factors that help protect infants from infections and diseases, reducing the risk of conditions such as respiratory infections and gastrointestinal diseases.
- Bonding: Breastfeeding promotes maternal-infant bonding, which is crucial for emotional and psychological development.
- Long-term Health Benefits: Studies indicate that breastfeeding is associated with a lower risk of obesity, diabetes, and certain chronic diseases in later life.
Recommendations: The World Health Organization (WHO) and the American Academy of Pediatrics (AAP) recommend exclusive breastfeeding for the first six months, followed by the introduction of complementary foods while continuing breastfeeding for at least one year or beyond.
Formula Feeding:

For mothers who cannot or choose not to breastfeed, infant formula is a safe and nutritious alternative. Modern formulas are designed to closely resemble breast milk and contain the necessary nutrients for infant growth and development.
Types of Formula:
- Cow’s Milk-Based Formula: The most common type, suitable for most infants.
- Soy-Based Formula: For infants with lactose intolerance or dairy allergies.
- Hydrolyzed Protein Formula: For infants with protein allergies; proteins are broken down into smaller components for easier digestion.
Alternatives to Breastfeeding: While breastfeeding is ideal, it is important to support parents in making informed choices about formula feeding. Guidance should include:
- Ensuring the formula is prepared and stored safely.
- Recognizing hunger cues and understanding feeding schedules.
- Consulting healthcare providers for personalized recommendations.
Introduction of Solids

Guidelines for Introducing Solid Foods: The introduction of solid foods typically begins around six months of age, when infants show readiness signs such as good head and neck control, the ability to sit with support, and the loss of the tongue-thrust reflex.
First Foods:
- Single-Grain Cereals: Iron-fortified rice or oatmeal cereals are excellent first foods.
- Pureed Fruits and Vegetables: Introduce one food at a time to monitor for allergies. Common options include pureed sweet potatoes, bananas, and apples.
- Protein Sources: Gradually incorporate pureed meats, beans, and later, finely chopped soft foods.
Advancing Solid Foods: As infants grow and develop their chewing skills, parents can introduce a variety of textures and flavors. By 12 months, most children can consume a wide range of family foods, transitioning from purees to soft table foods.
Mealtime Practices:
- Encourage a positive mealtime environment, avoiding pressure to eat.
- Aim for regular meal and snack times to establish routine.
- Promote self-feeding with appropriate utensils to foster independence.
Allergies and Intolerances: Introduce potential allergens (such as peanuts and eggs) early in the solid food introduction phase to reduce the risk of developing allergies, especially if there is a family history of allergies.
Growth Monitoring
Assessing Growth Patterns: Regular growth monitoring is essential in pediatric care to ensure that infants and children are developing appropriately. Growth is typically assessed using growth charts that plot weight, height, and head circumference against standardized percentiles.
Key Indicators:
- Weight for Age: Monitoring weight gain patterns helps identify undernutrition or obesity.
- Length for Age: Ensures that height is appropriate for age, indicating proper nutrition.
- Weight for Length: This measure helps assess body composition and detect issues like malnutrition or obesity.
Adjusting Nutritional Intake: Healthcare providers should work with families to adjust dietary intake based on growth assessments. This may involve increasing caloric intake for underweight infants or promoting healthy eating habits in overweight children.
Common Nutritional Issues
Iron Deficiency

Prevention and Management: Iron deficiency is a common nutritional issue in infants and children, particularly during periods of rapid growth. It can lead to anemia, affecting cognitive and physical development.
Risk Factors:
- Exclusively breastfeeding beyond six months without iron supplementation.
- Insufficient dietary intake of iron-rich foods.
- Low birth weight or prematurity.
Preventive Measures:
- For breastfed infants, introduce iron-rich foods (like pureed meats and iron-fortified cereals) around six months of age.
- Ensure that formula-fed infants receive iron-fortified formula.
Management: If iron deficiency is diagnosed, treatment may include:
- Dietary Changes: Increasing intake of iron-rich foods (red meats, legumes, fortified cereals).
- Iron Supplements: For diagnosed anemia, oral iron supplements may be prescribed under medical supervision. It’s crucial to monitor for side effects, such as gastrointestinal discomfort.
Obesity

Addressing Weight Management: Childhood obesity is a significant public health concern, linked to numerous health issues, including diabetes, hypertension, and psychological effects.
Contributing Factors:
- Poor dietary habits: High intake of sugary beverages and processed foods.
- Sedentary lifestyle: Limited physical activity due to screen time and lack of outdoor play.
- Socioeconomic factors: Limited access to healthy foods and safe environments for physical activity.
Strategies for Prevention and Management:
- Education: Teaching families about balanced diets, portion sizes, and the importance of physical activity.
- Encouraging Healthy Eating Habits: Promote fruits, vegetables, whole grains, and lean proteins while limiting processed foods and sugars.
- Physical Activity: Encourage at least 60 minutes of physical activity each day for children, incorporating fun and engaging activities.
- Family Involvement: Involve the entire family in making healthier lifestyle choices, creating a supportive environment.
Monitoring Progress: Regular follow-up appointments should assess changes in weight, dietary habits, and activity levels. Setting realistic, achievable goals is crucial for sustainable weight management.
Conclusion
In summary, understanding the nutritional needs of infants and children is vital for fostering healthy growth and development. From breastfeeding and formula feeding to the introduction of solid foods and addressing common nutritional issues, caregivers and healthcare providers must work together to ensure that children receive the best possible nutrition. This collaborative effort lays the foundation for a lifetime of healthy eating habits and optimal well-being.
Nutritional Needs Across the Lifespan: Adolescents
Adolescents

Adolescence is a critical period of growth and development, characterized by significant physical, emotional, and social changes. During this stage, individuals experience rapid growth spurts and increased physical activity, necessitating a comprehensive understanding of their nutritional needs. Proper nutrition during adolescence lays the foundation for a healthy adulthood and helps prevent long-term health issues.
Nutritional Needs
Increased Caloric Needs
Growth Spurts: Adolescence is marked by significant increases in height and weight, with most adolescents experiencing their largest growth spurt during this period. This growth varies between sexes and can occur as early as ages 10-12 for girls and 12-14 for boys. On average, boys may gain 10-12 inches in height and 40-50 pounds, while girls may gain 8-10 inches and 35-45 pounds.
Increased Physical Activity: As adolescents engage in sports, physical education, and recreational activities, their energy expenditure rises. Teenagers often participate in higher levels of physical activity, which, combined with growth spurts, leads to increased caloric needs.
Caloric Recommendations:
- Girls (ages 9-13): Approximately 1,600-2,200 calories per day, depending on activity level.
- Boys (ages 9-13): Approximately 1,800-2,600 calories per day, depending on activity level.
- Girls (ages 14-18): Approximately 1,800-2,400 calories per day.
- Boys (ages 14-18): Approximately 2,200-3,200 calories per day.
Sources of Calories: It’s essential that adolescents receive calories from a variety of nutrient-dense foods, including:
- Whole grains (e.g., brown rice, whole wheat bread)
- Lean proteins (e.g., poultry, fish, legumes)
- Healthy fats (e.g., avocados, nuts, olive oil)
- Fruits and vegetables to ensure they receive vitamins, minerals, and fiber.
Nutrient Requirements
Calcium:
Calcium is critical during adolescence for bone development and achieving peak bone mass. Most bone growth occurs during this period, making adequate calcium intake essential to reduce the risk of osteoporosis later in life.
- Recommended Intake:
- Ages 9-18: 1,300 mg per day.
- Sources of Calcium:
- Dairy products (milk, yogurt, cheese)
- Fortified plant-based milks (almond, soy)
- Leafy greens (kale, broccoli)
- Tofu and fortified foods (cereals, orange juice).
Iron:

Iron is vital for the development of hemoglobin and overall energy levels. Adolescents, especially girls, face increased iron needs due to menstruation and growth.
- Recommended Intake:
- Girls (ages 14-18): 15 mg per day.
- Boys (ages 14-18): 11 mg per day.
- Sources of Iron:
- Red meat, poultry, and fish (heme iron)
- Beans, lentils, tofu, and fortified cereals (non-heme iron).
- Vitamin C-rich foods (like citrus fruits) can enhance iron absorption when consumed alongside iron-rich foods.
Vitamins:
| Vitamin | Role | Food Sources |
| Vitamin A (Retinol) | Vision, immune function, skin health, cellular communication | Liver, fish oils, eggs, dairy, carrots, sweet potatoes, spinach, kale, mangoes |
| Vitamin B1 (Thiamine) | Carbohydrate metabolism, nerve function | Whole grains, pork, sunflower seeds, beans, peas |
| Vitamin B2 (Riboflavin) | Energy production, skin and vision health | Eggs, dairy, lean meats, leafy greens, almonds |
| Vitamin B3 (Niacin) | Digestion, skin health, energy conversion, cholesterol control | Meat, fish, poultry, whole grains, fortified cereals, peanuts |
| Vitamin B5 (Pantothenic Acid) | Fatty acid metabolism, hormone production | Avocados, yogurt, chicken, beef, mushrooms, sweet potatoes, eggs |
| Vitamin B6 (Pyridoxine) | Protein metabolism, neurotransmitter production, red blood cell formation | Poultry, fish, potatoes, chickpeas, bananas, fortified cereals |
| Vitamin B7 (Biotin) | Metabolism of fats, carbohydrates, proteins, hair and nail health | Eggs, almonds, spinach, sweet potatoes, salmon, seeds |
| Vitamin B9 (Folate/Folic Acid) | DNA synthesis, cell growth, red blood cell formation, fetal development | Leafy greens, legumes, fortified cereals, citrus fruits, liver |
| Vitamin B12 (Cobalamin) | Nerve function, red blood cell formation, DNA synthesis | Meat, fish, dairy, eggs, fortified plant-based milks, fortified cereals |
| Vitamin C (Ascorbic Acid) | Antioxidant, immune support, collagen synthesis, iron absorption | Citrus fruits, strawberries, kiwi, bell peppers, broccoli, tomatoes, spinach |
| Vitamin D | Calcium and phosphorus regulation, bone health, immune support | Sunlight, fatty fish (salmon, mackerel), fortified milk, cheese, egg yolks |
| Vitamin E (Tocopherol) | Antioxidant, cell protection, immune function, skin health | Nuts, seeds, vegetable oils (sunflower, safflower, olive oil), spinach, broccoli |
| Vitamin K | Blood clotting, bone health, calcium regulation | Leafy greens (kale, spinach, broccoli), Brussels sprouts, cabbage, liver, dairy products |
Dietary Concerns
Eating Disorders

Identification: Eating disorders are serious mental health conditions that can arise during adolescence. Common disorders include anorexia nervosa, bulimia nervosa, and binge-eating disorder. Signs may include:
- Significant weight loss or fluctuations.
- Preoccupation with food, dieting, and body image.
- Changes in eating habits (e.g., avoiding certain foods, extreme dieting).
- Physical symptoms (fatigue, dizziness, hair loss, and irregular menstrual cycles).
Management: Managing eating disorders requires a multidisciplinary approach involving healthcare professionals, including dietitians, therapists, and medical doctors.
- Therapeutic Approaches:
- Cognitive Behavioral Therapy (CBT) can be effective in treating eating disorders by helping individuals understand and change distorted thoughts and behaviors regarding food and body image.
- Nutritional counseling focuses on developing healthy eating patterns and addressing nutritional deficiencies.
- Family Support: Family involvement is crucial in treatment. Educating family members about eating disorders and fostering a supportive environment can aid recovery.
- Monitoring and Follow-Up: Regular follow-ups with healthcare providers are essential to track progress, make necessary dietary adjustments, and ensure physical health is maintained.
Fad Diets
Understanding Fad Diets: Fad diets often promise quick weight loss and can be appealing to adolescents seeking to fit in or meet societal beauty standards. However, many fad diets lack scientific backing and may pose health risks.
Common Fad Diets:
- Ketogenic Diet: High in fats and low in carbohydrates; may lead to nutrient deficiencies and is challenging to maintain.
- Intermittent Fasting: Involves cycling between eating and fasting; may not be suitable for adolescents who require consistent energy for growth and activity.
- Detox Diets: Often involve extreme restrictions and can lead to inadequate nutrient intake.
Risks of Fad Diets:
- Nutrient deficiencies, leading to fatigue, weakness, and compromised immune function.
- Disordered eating patterns that can lead to long-term health issues.
- Potential for yo-yo dieting, where weight fluctuates dramatically, increasing the risk of obesity.
Educating Adolescents:
- Promote balanced eating rather than extreme restrictions.
- Discuss the importance of long-term healthy eating habits over short-term weight loss.
- Encourage critical thinking about diet trends and the credibility of sources.
Conclusion
In conclusion, understanding the nutritional needs of adolescents is vital for promoting healthy growth and development during this formative period. Adolescents require increased caloric intake and specific nutrients such as calcium, iron, and vitamins to support their physical and cognitive development. Awareness of dietary concerns, including eating disorders and fad diets, is crucial for providing appropriate guidance and support. By fostering healthy eating habits and promoting a positive body image, healthcare providers can help adolescents navigate the challenges of nutrition during this critical stage of life.
Nutritional Needs Across the Lifespan: Adults
Adults

As individuals transition into adulthood, their nutritional needs evolve significantly. This stage of life is crucial for maintaining health, managing weight, and preventing chronic diseases. A well-balanced diet that meets macronutrient and micronutrient requirements is essential for optimal health. Furthermore, understanding the impact of lifestyle factors such as physical activity, stress, and sleep is vital in tailoring nutrition to individual needs.
Balanced Diet
A balanced diet is fundamental to achieving and maintaining good health. It involves consuming the right proportions of macronutrients and micronutrients that support bodily functions and energy needs.
Macronutrients
- Carbohydrates:
- Role: Carbohydrates are the body’s primary source of energy. They are crucial for fueling physical activity and supporting brain function.
- Types:
- Simple Carbohydrates: These include sugars found in fruits (fructose) and milk (lactose), as well as added sugars in processed foods. While they provide quick energy, excessive intake can lead to weight gain and metabolic issues.
- Complex Carbohydrates: Found in whole grains (brown rice, quinoa, oats), legumes, and starchy vegetables (sweet potatoes, corn), complex carbohydrates provide sustained energy and are rich in fiber, which supports digestive health and satiety.
- Recommended Intake: Carbohydrates should constitute about 45-65% of total daily caloric intake, emphasizing whole and minimally processed sources.
- Proteins:
- Role: Proteins are essential for growth, tissue repair, and the production of enzymes and hormones. They play a critical role in maintaining muscle mass and supporting immune function.
- Sources: High-quality protein sources include lean meats, poultry, fish, eggs, dairy products, legumes, nuts, and seeds. Plant-based proteins, such as beans and lentils, are also excellent choices, especially for those following vegetarian or vegan diets.
- Recommended Intake: The general recommendation for adults is about 10-35% of total daily calories from protein, with an emphasis on lean sources. A guideline is to consume 0.8 grams of protein per kilogram of body weight, but this may increase for athletes or those engaged in regular intense physical activity.
- Fats:
- Role: Fats are vital for hormone production, nutrient absorption (especially fat-soluble vitamins A, D, E, and K), and providing long-lasting energy. Healthy fats can improve heart health and support cognitive function.
- Types:
- Saturated Fats: Found in animal products (meat, butter, cheese) and some plant oils (coconut and palm oil), these should be limited to less than 10% of total daily calories to reduce the risk of heart disease.
- Unsaturated Fats: These include monounsaturated (olive oil, avocados) and polyunsaturated fats (fatty fish, flaxseeds). They are beneficial for heart health and should be included as part of a balanced diet.
- Recommended Intake: Fats should make up about 20-35% of total daily caloric intake, prioritizing unsaturated fats over saturated and trans fats.
Micronutrients
- Vitamins:
- Role: Vitamins are organic compounds that support various bodily functions, including metabolism, immune function, and cellular repair.
- Types:
- Water-soluble Vitamins: Includes vitamin C and B vitamins (B1, B2, B3, B5, B6, B7, B9, B12). These are not stored in the body and must be consumed regularly through a varied diet.
- Fat-soluble Vitamins: Includes vitamins A, D, E, and K. These are stored in body fat and the liver, allowing for greater variability in intake.
- Sources: A varied diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats typically provides adequate vitamins. Supplementation may be necessary in certain cases, such as with vitamin D in areas with limited sunlight.
- Minerals:
- Role: Minerals are inorganic substances necessary for various physiological functions, including bone health, nerve transmission, and fluid balance.
- Key Minerals:
- Calcium: Essential for bone health and muscle function. Recommended intake for adults is 1,000 mg per day, increasing to 1,200 mg for women over 50 and men over 70.
- Iron: Important for oxygen transport and energy metabolism. Adult men need about 8 mg daily, while women aged 19-50 require about 18 mg due to menstruation.
- Magnesium, Potassium, and Zinc: These minerals support muscle and nerve function, electrolyte balance, and immune health.
- Sources: A diet rich in fruits, vegetables, whole grains, nuts, seeds, and lean proteins will provide sufficient minerals. Specific populations (e.g., vegetarians, pregnant women) may require tailored dietary strategies.
Preventive Nutrition
Preventive nutrition focuses on maintaining health and preventing chronic diseases through dietary choices and lifestyle modifications. Chronic diseases such as obesity, diabetes, cardiovascular diseases, and certain cancers can often be mitigated through proper nutrition.
Strategies for Preventive Nutrition
- Maintain a Healthy Weight:

- Achieving and maintaining a healthy weight is crucial for reducing the risk of chronic diseases. A balanced diet combined with regular physical activity helps achieve this.
- Body Mass Index (BMI): While BMI is a useful screening tool, it should be used in conjunction with other assessments (like waist circumference and body composition) to evaluate health risks.
Limit Processed Foods:

- Highly processed foods are often high in added sugars, unhealthy fats, and sodium, contributing to weight gain and chronic disease risk. Encouraging whole foods, such as fruits, vegetables, and whole grains, can help promote better health outcomes.
Increase Fiber Intake:
-
- Dietary fiber plays a significant role in preventing constipation, lowering cholesterol levels, and reducing the risk of heart disease and type 2 diabetes. Adults should aim for 25-30 grams of fiber per day from whole foods.
- Sources of Fiber: Include whole grains, fruits, vegetables, legumes, nuts, and seeds.
2. Hydration:

- Staying hydrated is essential for overall health. Water is the best choice for hydration, while sugary drinks should be limited. Aim for at least 8 cups (64 ounces) of water per day, adjusting for activity level, climate, and individual needs.
3. Mindful Eating:
-
- Encouraging mindfulness in eating practices can help individuals recognize hunger cues, improve food choices, and prevent overeating. This includes focusing on meals without distractions and savoring the flavors and textures of food.
4. Regular Health Screenings:
-
- Routine health screenings (such as blood pressure checks, cholesterol levels, and blood glucose tests) can help identify risk factors for chronic diseases early on.
Lifestyle Factors
Lifestyle factors, including physical activity, stress management, and sleep quality, significantly influence nutritional needs and overall health.
Physical Activity

- Role in Health:
- Regular physical activity is essential for maintaining a healthy weight, improving cardiovascular health, and enhancing mental well-being. It can also reduce the risk of chronic diseases and improve metabolic health.
- The Centers for Disease Control and Prevention (CDC) recommends at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity activity each week, along with muscle-strengthening activities on two or more days.
- Nutrition and Exercise:
- Nutrition plays a critical role in supporting physical activity. Adequate carbohydrate intake provides energy for workouts, while protein aids in muscle recovery and growth.
- Hydration is also crucial before, during, and after exercise to prevent dehydration and optimize performance.
Stress Management
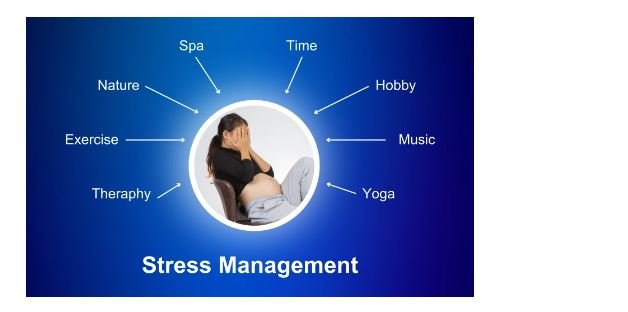
- Impact on Nutrition:
- Chronic stress can lead to emotional eating, where individuals may turn to food for comfort. This often results in the consumption of high-calorie, low-nutrient foods, contributing to weight gain and poor nutritional habits.
- Stress can also affect digestion and nutrient absorption, leading to gastrointestinal issues and further complicating nutritional needs.
- Stress-Reducing Strategies:
- Mindfulness practices, such as meditation and yoga, can help manage stress levels. Regular physical activity is also a powerful tool for stress reduction, as it releases endorphins that improve mood.
- Developing healthy coping mechanisms, such as engaging in hobbies, spending time with loved ones, and seeking professional help when needed, can further support emotional well-being.
Sleep

- Importance of Sleep:
- Quality sleep is essential for overall health, affecting metabolic health, appetite regulation, and cognitive function. Poor sleep is linked to obesity, diabetes, and cardiovascular diseases.
- Adults typically require 7-9 hours of sleep per night for optimal health.
- Nutrition and Sleep:
- Certain foods can promote better sleep quality. Foods rich in tryptophan (such as turkey, nuts, and seeds) can enhance serotonin levels, which help regulate sleep.
- Limiting caffeine and alcohol, particularly close to bedtime, is crucial as these substances can disrupt sleep patterns.
- Creating a Sleep-Friendly Environment:
- Establishing a regular sleep schedule, creating a comfortable sleeping environment, and limiting screen time before bed can improve sleep quality.
Conclusion
In conclusion, adults have unique nutritional needs that are essential for maintaining health and preventing chronic diseases. A balanced diet rich in macronutrients and micronutrients is vital for supporting bodily functions and energy levels. Preventive nutrition strategies can significantly reduce the risk of chronic illnesses, while lifestyle factors such as physical activity, stress management, and sleep quality further influence nutritional needs.
Nutritional Needs Across the Lifespan: Older Adults
As individuals age, their nutritional needs become increasingly complex due to a variety of physiological and lifestyle changes. Older adults often face unique challenges that can impact their overall health and well-being. Understanding age-related changes in metabolism, digestion, and nutrient absorption, as well as addressing specific nutritional challenges, is essential for promoting optimal health in this population.
Age-Related Changes
Metabolism
- Slower Basal Metabolic Rate (BMR):
- As individuals age, their BMR typically decreases, meaning the body requires fewer calories to maintain basic physiological functions. This decline is influenced by several factors, including loss of lean body mass and hormonal changes.
- Impact on Nutrition: Older adults may need to adjust their caloric intake to prevent weight gain while ensuring they receive sufficient nutrients. A focus on nutrient-dense foods is critical to meet their needs without exceeding caloric limits.
- Changes in Hormonal Regulation:
- Hormonal shifts, particularly in insulin and glucagon levels, can affect glucose metabolism and energy balance. Insulin sensitivity may decrease, leading to challenges in blood sugar management.
- Dietary Considerations: Carbohydrate intake should be carefully managed, with an emphasis on complex carbohydrates that provide fiber and support stable blood sugar levels.
Digestion
- Gastrointestinal Changes:
- Aging is associated with alterations in gastrointestinal function, including decreased gastric acid production, slower gastric emptying, and reduced enzyme secretion. These changes can lead to decreased appetite and impaired digestion.
- Nutritional Strategy: Older adults may benefit from smaller, more frequent meals that are easier to digest. Including digestive enzymes and probiotic-rich foods can also support gastrointestinal health.
- Alterations in Taste and Smell:
- Many older adults experience changes in taste and smell, which can diminish appetite and affect food preferences. This can lead to decreased food intake and, consequently, nutrient deficiencies.
- Approach to Enhancing Flavor: Incorporating herbs and spices can enhance the taste of foods without relying on excessive salt or sugar. Texture modifications, such as softer foods, can also make meals more appealing.
Nutrient Absorption
- Decreased Nutrient Absorption:
- Age-related changes can impair nutrient absorption in the intestines. For example, the absorption of vitamin B12 may be compromised due to reduced stomach acid, and calcium absorption may also decline.
- Nutritional Solutions: Older adults may require fortified foods or supplements to meet their nutrient needs, particularly for vitamins B12 and D, calcium, and magnesium.
- Increased Nutritional Needs:
- Despite reduced caloric needs, the requirement for certain nutrients, such as calcium, vitamin D, and protein, often increases in older adults to support bone health and muscle maintenance.
- Dietary Focus: Emphasizing nutrient-rich foods, including dairy products, leafy greens, and lean proteins, can help meet these increased needs.
Nutritional Challenges
Hydration
- Importance of Adequate Fluid Intake:
- Hydration is crucial for maintaining health and preventing complications such as urinary tract infections, constipation, and kidney stones. However, older adults often have a decreased thirst sensation, which can lead to inadequate fluid intake.
- Recommended Fluid Intake: Older adults should aim for at least 8-10 cups (64-80 ounces) of fluids per day, adjusting for climate, physical activity, and individual health conditions.
- Signs of Dehydration:
- Symptoms of dehydration can be subtle in older adults, including dry mouth, fatigue, dizziness, and confusion. Regular monitoring and proactive measures to encourage fluid intake are essential.
- Strategies to Promote Hydration: Providing accessible fluids, encouraging water-rich foods (such as fruits and vegetables), and offering beverages that are appealing can help maintain adequate hydration levels.
- Managing Fluid Intake with Chronic Conditions:
- Conditions such as heart failure or kidney disease may necessitate fluid restrictions. In such cases, it’s crucial to work with healthcare providers to develop individualized hydration plans that balance health needs with fluid intake.
Dental Issues

- Adapting Diets for Dental Problems:
- Dental health issues, such as tooth decay, gum disease, and loss of teeth, can significantly impact an older adult’s ability to chew and enjoy a variety of foods. This can lead to reduced nutrient intake and increased reliance on softer, less nutritious foods.
- Dietary Modifications: Incorporating soft foods, pureed items, and smoothies can help maintain nutritional intake while accommodating chewing difficulties.
- Nutritional Consequences of Dental Problems:
- A limited diet may increase the risk of deficiencies in essential nutrients, such as calcium, vitamin D, and protein. Older adults with dental issues may also be more prone to malnutrition and unintentional weight loss.
- Encouraging Dental Health: Regular dental check-ups and proper oral hygiene practices are critical in preventing dental problems and ensuring continued access to a varied diet.
- Supplementing Nutritional Needs:
- For individuals with significant dental issues, nutritional supplements (such as protein shakes or meal replacements) can help bridge the gap in nutrient intake and prevent deficiencies.
Chronic Conditions
1. Osteoporosis:
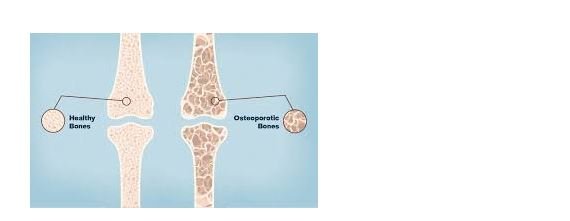
- Osteoporosis is a common condition in older adults characterized by reduced bone density and increased fracture risk. Nutritional management is vital for bone health.
- Calcium and Vitamin D: Adequate calcium intake (1,200 mg/day for women over 50 and men over 70) and vitamin D (800-1,000 IU/day) are crucial for bone health. Foods rich in calcium include dairy products, leafy greens, and fortified foods.
- Weight-Bearing Exercise: In conjunction with nutrition, engaging in weight-bearing exercises can help maintain bone density and reduce the risk of falls and fractures.
2. Diabetes:

- The prevalence of type 2 diabetes increases with age, making dietary management essential. Nutrition plays a significant role in blood sugar control and overall health.
- Carbohydrate Management: Older adults with diabetes should focus on managing carbohydrate intake, prioritizing whole grains, fruits, and vegetables, while monitoring portion sizes.
- Healthy Fats and Proteins: Incorporating healthy fats (such as those from fish, nuts, and olive oil) and lean proteins can help maintain blood sugar levels and support overall health.
3.0Heart Disease:

- Heart disease remains a leading cause of morbidity and mortality in older adults. Nutrition can help mitigate risk factors associated with cardiovascular diseases.
- Heart-Healthy Diet: A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can promote heart health. Limiting saturated fats, trans fats, and sodium is also crucial.
- Omega-3 Fatty Acids: Including sources of omega-3 fatty acids, such as fatty fish (salmon, mackerel) and flaxseeds, can help support cardiovascular health.
- Managing Multiple Chronic Conditions:
- Many older adults live with multiple chronic conditions, complicating dietary management. A personalized nutrition plan that considers all health conditions is essential for promoting optimal health.
- Collaborative Care: Working with a registered dietitian can help create an individualized dietary plan that addresses the unique needs of older adults with chronic conditions.
Conclusion
In conclusion, older adults face a range of nutritional challenges that arise from age-related changes in metabolism, digestion, and nutrient absorption. Addressing these challenges through careful dietary management and awareness of specific health conditions is vital for promoting health and well-being in this population.
Adequate hydration, attention to dental health, and the management of chronic conditions through nutrition are critical components of care for older adults. By fostering a holistic approach that encompasses dietary choices, lifestyle modifications, and regular health monitoring, healthcare providers can empower older adults to maintain their health, enhance their quality of life, and prevent the onset of nutrition-related issues.
