PN: Common Pediatric Illnesses and Conditions
-
Respiratory Disorders
Upper Respiratory Infections
-
Common Cold:

- Etiology: The common cold is primarily caused by viruses, including rhinoviruses, coronaviruses, and respiratory syncytial virus (RSV). It is highly contagious and spreads through respiratory droplets and direct contact.
- Symptoms: Symptoms typically include a runny or stuffy nose, sore throat, cough, mild fever, and general malaise. In infants and young children, symptoms may also include irritability and feeding difficulties.
- Diagnosis: Diagnosis is usually clinical, based on the history and physical examination. In some cases, rapid viral tests may be used to rule out other infections.
- Management and Nursing Care:
- Supportive Care: Encourage fluid intake, rest, and proper nutrition. Use saline nasal drops or a humidifier to relieve nasal congestion.
- Medication: Over-the-counter medications such as acetaminophen or ibuprofen can be used to alleviate fever and discomfort. Avoid the use of cough and cold medications in young children unless prescribed by a healthcare provider.
-
Croup:
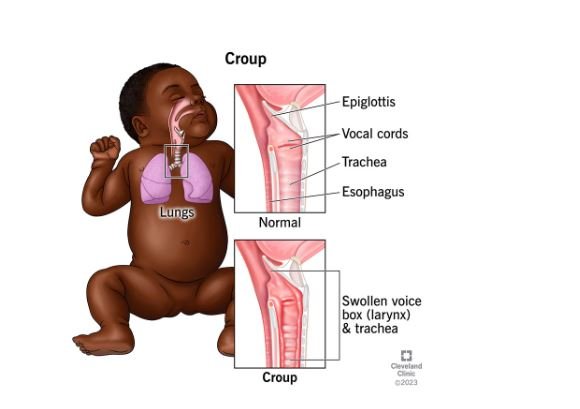
- Etiology: Croup is commonly caused by parainfluenza viruses, although other viruses can also be responsible. It is characterized by inflammation of the upper airways.
- Symptoms: Classic symptoms include a “barking” cough, stridor (a high-pitched wheezing sound), and hoarseness. Symptoms often worsen at night and can be accompanied by fever.
- Diagnosis: Diagnosis is primarily clinical. Severe cases may require imaging (e.g., neck X-ray) to confirm the presence of subglottic narrowing.
- Management and Nursing Care:
- Medications: Corticosteroids, such as dexamethasone, are commonly used to reduce inflammation. In severe cases, nebulized epinephrine may be administered.
- Supportive Measures: Ensure the child remains calm and comfortable. Cool mist from a humidifier or a cool evening air may help alleviate symptoms. Monitor for signs of respiratory distress and ensure adequate hydration.
-
Sinusitis:
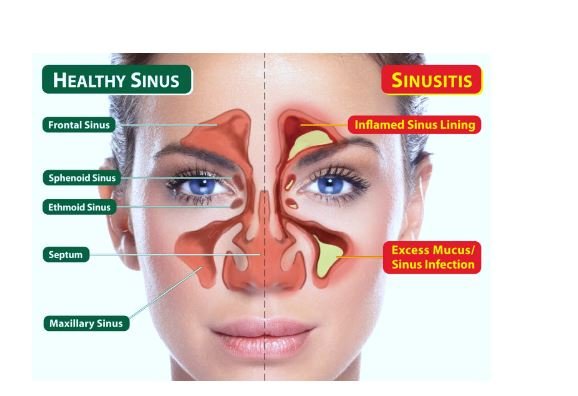
- Etiology: Sinusitis often follows a viral upper respiratory infection but can also be caused by bacterial or fungal infections. It involves inflammation of the sinuses.
- Symptoms: Symptoms include nasal congestion, facial pain or pressure, purulent nasal discharge, cough, and sometimes fever.
- Diagnosis: Diagnosis is based on clinical presentation and may be supported by imaging studies, such as sinus X-rays or CT scans, if symptoms are severe or persistent.
- Management and Nursing Care:
- Medications: Intranasal corticosteroids and saline nasal sprays can help reduce inflammation and improve sinus drainage. Antibiotics may be prescribed if a bacterial infection is suspected.
- Supportive Care: Encourage fluid intake and use a humidifier to help keep the nasal passages moist. Warm compresses can be applied to the face to alleviate discomfort.
Lower Respiratory Infections
-
Bronchiolitis:
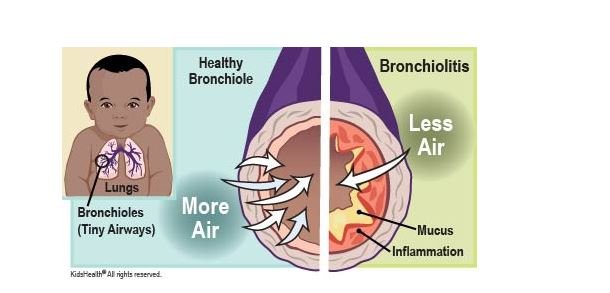
- Etiology: Bronchiolitis is commonly caused by RSV, particularly in infants. It involves inflammation and congestion in the small airways (bronchioles).
- Symptoms: Symptoms include wheezing, cough, respiratory distress, and sometimes fever. Infants may exhibit signs of difficulty breathing, such as nasal flaring or retractions.
- Diagnosis: Diagnosis is based on clinical presentation and may be supported by RSV testing or chest X-ray to rule out other conditions.
- Management and Nursing Care:
- Supportive Care: Ensure adequate hydration and monitor for signs of dehydration. Use a humidifier or provide humidified oxygen if needed.
- Medications: In severe cases, bronchodilators or corticosteroids may be administered. Ribavirin is reserved for high-risk infants in certain situations.
- Monitoring: Continuous monitoring of respiratory status and oxygen saturation is crucial. Provide education on signs of worsening and when to seek medical help.
-
Pneumonia:
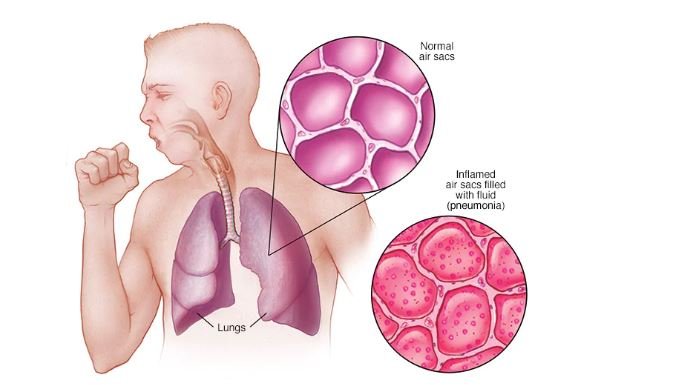
- Etiology: Pneumonia can be caused by a variety of pathogens, including bacteria (e.g., Streptococcus pneumoniae), viruses (e.g., influenza virus), and fungi.
- Symptoms: Symptoms include cough, fever, difficulty breathing, chest pain, and sometimes vomiting or abdominal pain.
- Diagnosis: Diagnosis involves clinical evaluation and may include imaging studies (e.g., chest X-ray) and laboratory tests to identify the causative agent.
- Management and Nursing Care:
- Medications: Antibiotics or antivirals may be prescribed depending on the causative pathogen. Ensure proper dosage and adherence.
- Supportive Care: Provide adequate hydration, rest, and fever management. Use a humidifier or administer oxygen therapy if necessary.
- Monitoring: Regularly monitor respiratory status, oxygen saturation, and signs of complications such as pleural effusion or lung abscess.
-
Asthma:
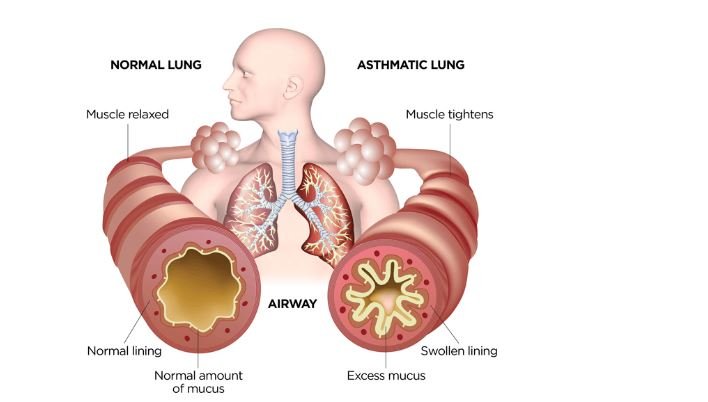
- Etiology: Asthma is a chronic inflammatory disease of the airways, often triggered by allergens, respiratory infections, or environmental factors.
- Symptoms: Symptoms include wheezing, cough, shortness of breath, and chest tightness. Symptoms can be intermittent or persistent and may vary in severity.
- Diagnosis: Diagnosis is based on clinical history, physical examination, and pulmonary function tests (e.g., spirometry). Allergy testing may also be conducted.
- Management and Nursing Care:
- Medications: Management includes both long-term control medications (e.g., inhaled corticosteroids) and quick-relief medications (e.g., bronchodilators). Educate on proper inhaler technique and medication adherence.
- Environmental Control: Identify and avoid asthma triggers. Implement measures such as using air purifiers, avoiding smoke, and managing allergies.
- Monitoring: Regularly monitor asthma control using peak flow meters and maintain a symptom diary. Educate families on recognizing signs of worsening asthma and the appropriate use of medications.
Management and Nursing Care for Respiratory Disorders
- Medication Administration: Ensure proper administration of medications, including dosing, timing, and technique. Educate caregivers on medication use and possible side effects.
- Respiratory Therapies: Implement therapies such as nebulized medications, chest physiotherapy, and supplemental oxygen as needed. Monitor effectiveness and adjust treatment plans based on the child’s response.
- Monitoring: Regularly monitor vital signs, respiratory status, and response to treatments. Use tools such as pulse oximeters to assess oxygen saturation and track progress.
-
Infectious Diseases
Viral Infections
-
Influenza:
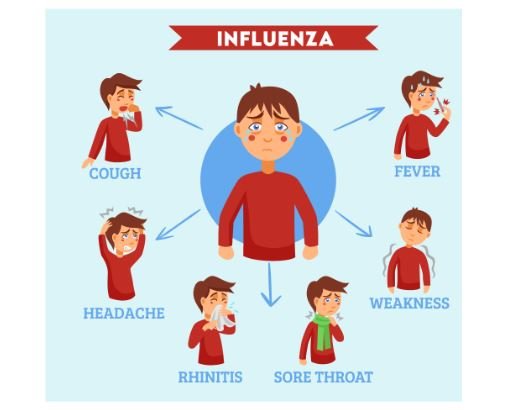
- Etiology: Influenza is caused by influenza viruses (types A and B). It spreads through respiratory droplets and can lead to seasonal outbreaks.
- Symptoms: Symptoms include high fever, chills, cough, sore throat, muscle aches, and fatigue. Gastrointestinal symptoms may also occur, particularly in younger children.
- Diagnosis: Diagnosis is often clinical but can be confirmed with rapid influenza diagnostic tests (RIDTs) or PCR tests.
- Management and Nursing Care:
- Medications: Antiviral medications such as oseltamivir (Tamiflu) may be prescribed to reduce the severity and duration of symptoms if given early in the course of illness.
- Supportive Care: Encourage rest, fluid intake, and fever management with acetaminophen or ibuprofen. Implement infection control measures to prevent spread.
- Vaccination: Annual influenza vaccination is recommended for all children aged 6 months and older to prevent influenza and its complications.
-
Chickenpox (Varicella):

- Etiology: Chickenpox is caused by the varicella-zoster virus (VZV). It spreads through respiratory droplets and direct contact with vesicular lesions.
- Symptoms: Symptoms include an itchy rash with red spots that develop into fluid-filled blisters, fever, and malaise.
- Diagnosis: Diagnosis is based on clinical presentation and history of exposure. Laboratory tests, including PCR or direct fluorescent antibody testing, may be used in uncertain cases.
- Management and Nursing Care:
- Medications: Antiviral medications, such as acyclovir, may be used in severe cases or for high-risk individuals. Antihistamines can help alleviate itching.
- Supportive Care: Provide comfort measures such as oatmeal baths and calamine lotion to soothe itching. Encourage hydration and rest.
- Vaccination: Varicella vaccination is recommended for children to prevent chickenpox and reduce the risk of complications.
-
Measles:

- Etiology: Measles is caused by the measles virus and is transmitted via respiratory droplets. It is highly contagious.
- Symptoms: Symptoms include high fever, cough, coryza, conjunctivitis, and a characteristic rash that starts on the face and spreads downward.
- Diagnosis: Diagnosis is based on clinical presentation and may be confirmed with serologic testing for measles-specific IgM antibodies or PCR testing.
- Management and Nursing Care:
- Medications: No specific antiviral treatment for measles. Vitamin A supplementation may be recommended in some cases to reduce complications.
- Supportive Care: Manage fever with acetaminophen or ibuprofen, and ensure adequate hydration and rest. Implement isolation precautions to prevent spread.
- Vaccination: The measles, mumps, and rubella (MMR) vaccine is recommended for all children to prevent measles and its complications.
Bacterial Infections
-
Streptococcal Infections:
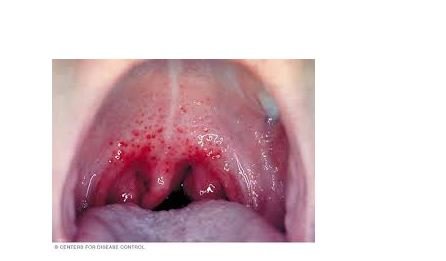
- Etiology: Streptococcal infections are caused by Group A Streptococcus (GAS). Common manifestations include pharyngitis (strep throat) and impetigo.
- Symptoms: Symptoms of strep throat include sore throat, fever, and swollen lymph nodes. Impetigo presents with red sores that ooze and form honey-colored crusts.
- Diagnosis: Diagnosis is based on clinical presentation and can be confirmed with throat cultures or rapid strep tests.
- Management and Nursing Care:
- Medications: Antibiotic therapy, typically penicillin or amoxicillin, is used to treat streptococcal infections. Ensure full adherence to the prescribed course.
- Supportive Care: Provide symptomatic relief, such as pain management and hydration. Practice good hygiene to prevent the spread of infection.
- Follow-up: Monitor for potential complications, such as rheumatic fever or glomerulonephritis, and ensure completion of the antibiotic course.
-
Pertussis (Whooping Cough):

- Etiology: Pertussis is caused by Bordetella pertussis. It is characterized by severe coughing fits followed by a “whooping” sound.
- Symptoms: Symptoms include a paroxysmal cough, post-tussive vomiting, and a whooping sound during inhalation. The cough may persist for weeks to months.
- Diagnosis: Diagnosis is confirmed through PCR testing of nasal secretions or a culture of the bacterium.
- Management and Nursing Care:
- Medications: Antibiotic treatment, such as azithromycin or erythromycin, is used to shorten the duration of symptoms and reduce transmission.
- Supportive Care: Provide supportive care, including hydration and cough management. Implement isolation precautions to prevent spread.
- Vaccination: The DTaP vaccine is recommended for children to prevent pertussis. Booster doses may be needed for older children and adults.
-
Tuberculosis (TB):
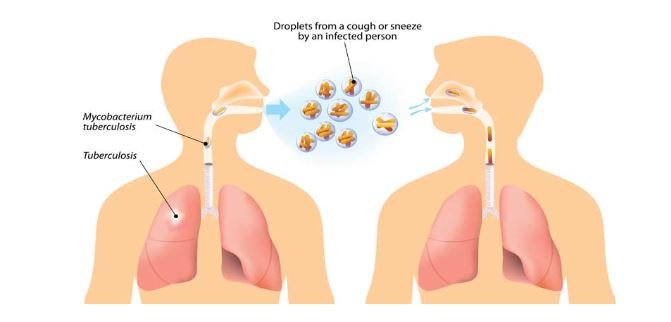
- Etiology: Tuberculosis is caused by Mycobacterium tuberculosis and primarily affects the lungs. It is transmitted through airborne droplets.
- Symptoms: Symptoms include persistent cough, fever, night sweats, weight loss, and hemoptysis (coughing up blood).
- Diagnosis: Diagnosis is confirmed with a combination of tuberculin skin tests (TST), chest X-rays, and sputum cultures.
- Management and Nursing Care:
- Medications: TB treatment involves a regimen of multiple antibiotics, including isoniazid, rifampin, ethambutol, and pyrazinamide. Ensure adherence to the full course to prevent drug resistance.
- Supportive Care: Monitor for side effects of medications and provide education on TB transmission and infection control measures.
- Isolation Precautions: Implement airborne precautions to prevent the spread of TB to others.
Management and Nursing Care for Infectious Diseases
- Isolation Precautions: Implement appropriate isolation precautions based on the type of infectious disease (e.g., droplet, contact, airborne). Educate families on infection control measures to prevent transmission.
- Antibiotic Therapy: Ensure correct administration of antibiotics, including dosage, frequency, and duration. Monitor for adverse reactions and provide education on completing the full course of treatment.
- Supportive Care: Provide symptomatic relief, such as fever management, hydration, and rest. Ensure the comfort and safety of the child and monitor for signs of complications.
-
Other Common Conditions
Gastrointestinal Issues
-
Gastroenteritis:
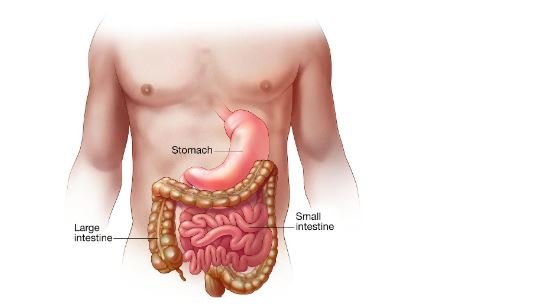
- Etiology: Gastroenteritis can be caused by viral (e.g., rotavirus), bacterial (e.g., Salmonella), or parasitic (e.g., Giardia) infections. It leads to inflammation of the stomach and intestines.
- Symptoms: Symptoms include diarrhea, vomiting, abdominal pain, and sometimes fever. Dehydration is a significant concern.
- Diagnosis: Diagnosis is based on clinical presentation and may include stool cultures, electrolyte panels, and other diagnostic tests.
- Management and Nursing Care:
- Hydration: Administer oral rehydration solutions (ORS) to replace lost fluids and electrolytes. Monitor for signs of dehydration, such as decreased urine output and dry mucous membranes.
- Dietary Management: Introduce a bland diet as tolerated, such as BRAT (bananas, rice, applesauce, toast) foods. Avoid dairy products and sugary beverages.
- Monitoring: Track fluid intake and output, and monitor for complications such as severe dehydration or electrolyte imbalances.
-
Constipation:
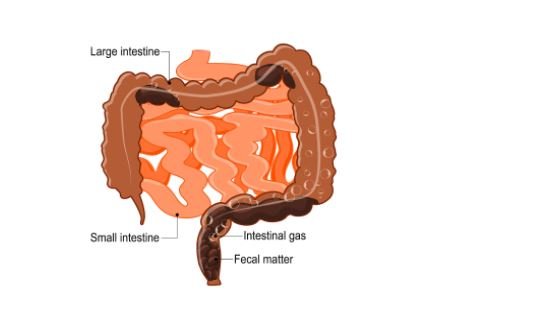
- Etiology: Constipation can be due to dietary factors, dehydration, lack of physical activity, or underlying medical conditions.
- Symptoms: Symptoms include infrequent bowel movements, hard stools, abdominal discomfort, and straining during defecation.
- Diagnosis: Diagnosis is based on clinical history and physical examination. In some cases, abdominal X-rays or other imaging studies may be needed.
- Management and Nursing Care:
- Dietary Interventions: Increase fiber intake with fruits, vegetables, and whole grains. Encourage adequate fluid consumption.
- Medications: Use stool softeners or laxatives as needed. Ensure proper dosing and monitor for side effects.
- Behavioral Strategies: Encourage regular toilet habits and physical activity to promote regular bowel movements.
-
Reflux (Gastroesophageal Reflux Disease, GERD):

- Etiology: GERD occurs when stomach acid frequently flows back into the esophagus, causing irritation and discomfort.
- Symptoms: Symptoms include regurgitation, vomiting, coughing, irritability, and feeding difficulties.
- Diagnosis: Diagnosis may involve clinical evaluation, pH monitoring, and endoscopy to assess the severity of reflux.
- Management and Nursing Care:
- Dietary Management: Offer smaller, more frequent feedings and avoid spicy or acidic foods. Elevate the head of the bed during sleep.
- Medications: Use antacids, H2-receptor antagonists, or proton pump inhibitors as prescribed. Educate on proper medication administration and possible side effects.
- Monitoring: Track symptoms and monitor for potential complications such as esophagitis or respiratory issues.
Dermatologic Conditions
-
Eczema (Atopic Dermatitis):

- Etiology: Eczema is a chronic inflammatory skin condition often associated with a family history of atopy (asthma, allergic rhinitis). It is characterized by dry, itchy, and inflamed skin.
- Symptoms: Symptoms include itching, redness, and rash, typically affecting the cheeks, arms, and legs. Secondary infections may occur due to scratching.
- Diagnosis: Diagnosis is based on clinical presentation and history. Skin biopsy is rarely needed but may be performed in atypical cases.
- Management and Nursing Care:
- Skin Care: Use emollients and moisturizers to maintain skin hydration. Avoid known irritants and allergens. Implement bathing routines using mild, non-soap cleansers.
- Medications: Apply topical corticosteroids or calcineurin inhibitors as prescribed. Monitor for side effects and provide education on proper application techniques.
- Education: Educate families on managing triggers and implementing skin care routines to prevent flare-ups.
-
Impetigo:

- Etiology: Impetigo is a highly contagious bacterial skin infection usually caused by Staphylococcus aureus or Streptococcus pyogenes. It is characterized by honey-colored crusted lesions.
- Symptoms: Symptoms include red sores that rupture, ooze, and form a yellow-brown crust. The infection often begins around the nose and mouth.
- Diagnosis: Diagnosis is based on clinical appearance and may be confirmed with skin cultures.
- Management and Nursing Care:
- Medications: Use topical antibiotics (e.g., mupirocin) for localized infections. Oral antibiotics may be needed for more widespread cases.
- Hygiene: Implement good hand hygiene and wound care. Avoid sharing personal items and ensure that affected areas are kept clean and covered.
- Monitoring: Monitor for signs of complications or secondary infections and educate caregivers on preventing spread.
-
Scabies:

- Etiology: Scabies is caused by the mite Sarcoptes scabiei, which burrows into the skin and causes intense itching.
- Symptoms: Symptoms include itching, rash, and small red bumps, typically found in areas such as the wrists, elbows, and between the fingers.
- Diagnosis: Diagnosis is based on clinical presentation and can be confirmed by identifying mites or eggs through skin scrapings.
- Management and Nursing Care:
- Medications: Treat with topical scabicides, such as permethrin cream or ivermectin. Follow instructions for application and duration of treatment.
- Hygiene: Wash all bedding, clothing, and personal items in hot water to remove mites and prevent reinfestation.
- Education: Educate families about transmission, treatment, and prevention of scabies.
Neurological Conditions
-
Seizures:
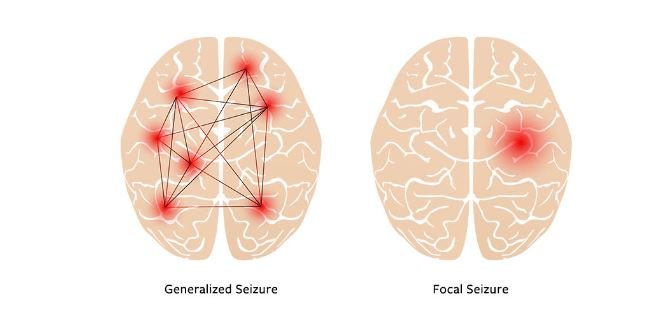
- Etiology: Seizures in children can be caused by various factors, including epilepsy, fever (febrile seizures), or metabolic disturbances.
- Symptoms: Symptoms vary depending on the type of seizure but may include loss of consciousness, convulsions, muscle rigidity, and altered behavior.
- Diagnosis: Diagnosis involves a thorough history, physical examination, and may include EEG, CT scans, or MRI.
- Management and Nursing Care:
- Medications: Antiepileptic drugs (AEDs) are used to manage seizures. Monitor for effectiveness and side effects.
- Safety: Implement safety measures to prevent injury during a seizure. Ensure proper positioning and monitoring.
- Education: Provide education on seizure recognition, first aid, and medication adherence. Encourage families to keep a seizure diary.
-
Migraine Headaches:
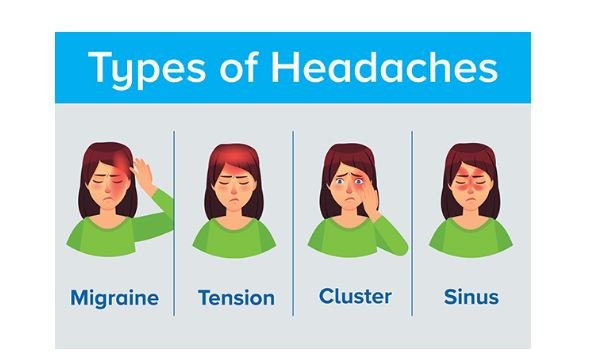
- Etiology: Migraines are severe headaches often associated with nausea, vomiting, and sensitivity to light or sound. They may have a genetic component.
- Symptoms: Symptoms include throbbing pain, often localized to one side of the head, accompanied by visual or gastrointestinal disturbances.
- Diagnosis: Diagnosis is based on clinical history and exclusion of other potential causes of headaches.
- Management and Nursing Care:
- Medications: Use medications such as NSAIDs or triptans for acute relief. Consider preventive medications for frequent migraines.
- Lifestyle Modifications: Identify and avoid migraine triggers, such as certain foods or stress. Encourage regular sleep patterns and hydration.
- Education: Educate families on recognizing migraine symptoms, managing triggers, and implementing lifestyle changes to reduce the frequency of headaches.
-
Chronic Conditions
Diabetes Mellitus
-
Type 1 Diabetes:
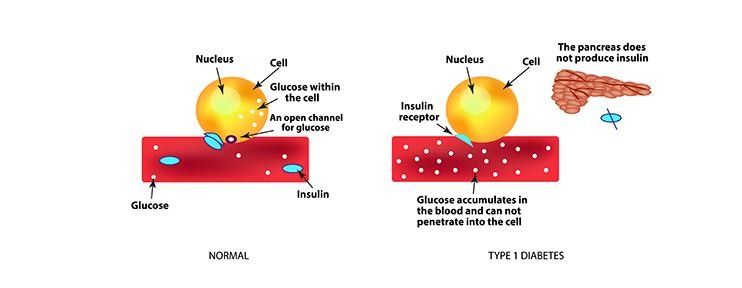
- Etiology: Type 1 diabetes is an autoimmune condition where the pancreas produces little to no insulin. It typically presents in childhood or adolescence.
- Symptoms: Symptoms include frequent urination, excessive thirst, unexplained weight loss, and fatigue.
- Diagnosis: Diagnosis is based on blood glucose tests, including fasting glucose, HbA1c, and oral glucose tolerance tests.
- Management and Nursing Care:
- Insulin Administration: Teach insulin administration techniques, including injection sites, dosage, and timing. Monitor blood glucose levels regularly.
- Dietary Management: Provide guidance on carbohydrate counting and meal planning to manage blood glucose levels. Work with a dietitian for individualized plans.
- Education: Educate families on recognizing and managing hypo- and hyperglycemia, and provide support for insulin pump or continuous glucose monitoring systems.
Cystic Fibrosis
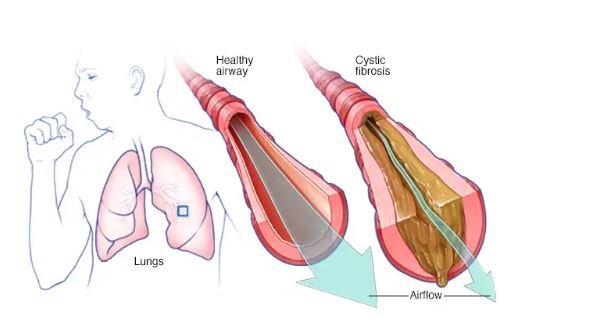
- Etiology: Cystic fibrosis is a genetic disorder affecting the CFTR gene, leading to thick mucus production that impacts the respiratory and digestive systems.
- Symptoms: Symptoms include chronic cough, frequent lung infections, poor weight gain, and digestive issues such as steatorrhea (fatty stools).
- Diagnosis: Diagnosis is confirmed through sweat chloride testing, genetic testing, and clinical evaluation.
- Management and Nursing Care:
- Airway Clearance Techniques: Implement therapies such as chest physiotherapy, positive expiratory pressure (PEP) devices, and nebulized medications to clear mucus from the lungs.
- Enzyme Replacement Therapy: Administer pancreatic enzyme supplements to aid in digestion and nutrient absorption. Monitor for effectiveness and adjust dosages as needed.
- Supportive Care: Provide nutritional support, including high-calorie diets and vitamin supplements. Monitor for complications such as lung infections and diabetes.
This comprehensive approach to pediatric nursing for common illnesses and conditions will ensure that the care provided is thorough, evidence-based, and tailored to the needs of children and their families.
