Dosage Calculations and Administration
Dosage Calculations and Administration
1. Dosage Calculations
Dosage Calculations and Administration
Dosage calculations are a critical aspect of nursing pharmacology, ensuring the safe and effective administration of medications. Nurses must accurately calculate dosages based on various factors, such as patient weight, body surface area, and medication concentration. This chapter will delve into the fundamentals of dosage calculations, including basic conversions, medication orders, and infusion rate calculations.
Basic Calculations
Conversions
Nurses frequently encounter medications in different units of measurement. Therefore, proficiency in metric conversions is essential. Common conversions include:
- milligrams (mg) to grams (g): 1 g = 1000 mg
- grams (g) to kilograms (kg): 1 kg = 1000 g
- milliliters (mL) to liters (L): 1 L = 1000 mL
Example: Convert 500 mg to grams.
Solution: 500 mg ÷ 1000 mg/g = 0.5 g
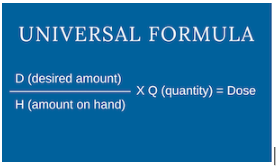
Dose Calculation
Dosage calculations often involve determining the appropriate amount of medication to administer based on the patient’s weight or body surface area.
Weight-based dosing:
Many medications are dosed based on the patient’s weight in kilograms (kg). The formula for weight-based dosing is:
Desired dose (mg/kg) × Patient weight (kg) = Total dose (mg)
Example: A patient weighing 75 kg is prescribed a medication at a dose of 10 mg/kg. Calculate the total dose.
Solution: 10 mg/kg × 75 kg = 750 mg
Body surface area (BSA)-based dosing:
Some medications, particularly those with a narrow therapeutic index, are dosed based on the patient’s BSA. The BSA can be estimated using various formulas, such as the:
Mosteller formula:
BSA (m²) = √(Height (cm) × Weight (kg)) / 3600
Once the BSA is calculated, the desired dose is determined using the prescribed dose per square meter (m²) of BSA.
Example: A patient with a BSA of 1.75 m² is prescribed a medication at a dose of 5 mg/m². Calculate the total dose.
Solution: 5 mg/m² × 1.75 m² = 8.75 mg
Medication Orders
Medication orders provide essential information about the prescribed medication, including the dose, route of administration, frequency, and duration of therapy. Nurses must carefully interpret medication orders to ensure accurate administration.
Volume and Concentration
Many medications are supplied in various concentrations. Nurses must calculate the appropriate volume to administer based on the desired dose and the concentration of the medication. The formula for calculating volume is:
Desired dose (mg) / Concentration (mg/mL) = Volume (mL)
Example: An order for 250 mg of a medication is available in a concentration of 500 mg/mL. Calculate the volume to administer.
Solution: 250 mg / 500 mg/mL = 0.5 mL
IV Drip Rates

Intravenous (IV) medications are often administered at a specific rate, measured in drops per minute (gtt/min) or milliliters per hour (mL/hr). The calculation of IV drip rates depends on the drop factor of the IV tubing and the desired infusion rate.
Drop factor: The drop factor indicates the number of drops in 1 mL of fluid. Common drop factors are 10, 15, 20, and 60 drops/mL.
Calculation of IV drip rate (gtt/min):
IV drip rate (gtt/min) = Volume (mL/hr) × Drop factor (drops/mL) / 60 min/hr
Example: Calculate the IV drip rate for a 1000 mL infusion over 8 hours using tubing with a drop factor of 15 drops/mL.
Solution: IV drip rate (gtt/min) = (1000 mL / 8 hr) × 15 drops/mL / 60 min/hr = 31.25 gtt/min
Calculation of IV drip rate (mL/hr):
IV drip rate (mL/hr) = Volume (mL) / Infusion time (hr)
Example: Calculate the IV drip rate for a 500 mL infusion over 4 hours.
Solution: IV drip rate (mL/hr) = 500 mL / 4 hr = 125 mL/hr
Additional Considerations
- Always double-check calculations with another nurse or pharmacist to prevent errors.
- Consider the patient’s age, weight, and renal or hepatic function when calculating dosages.
- Be aware of any contraindications or precautions associated with the medication.
- Monitor the patient’s response to the medication and adjust the dosage as needed.
By mastering dosage calculations and understanding the principles of medication administration, nurses can play a vital role in ensuring patient safety and optimizing treatment outcomes.
Administration Routes
Understanding various medication administration routes is crucial for effective pharmacotherapy. Each route has specific techniques, advantages, and considerations. This comprehensive guide covers oral, topical, parenteral, and inhalational routes, including detailed information on each.
1. Oral Administration
Oral administration is the most common and convenient route for drug delivery. It involves the ingestion of medication through the mouth. Medications administered orally are absorbed through the gastrointestinal (GI) tract.
a) Tablets

i. Types of Tablets:
- Standard Tablets: These are solid forms of medication designed to be swallowed whole.
- Chewable Tablets: Designed to be chewed before swallowing, often used for pediatric or geriatric patients.
- Extended-Release Tablets: These are formulated to release medication slowly over time, providing a prolonged therapeutic effect.
ii. Administration Considerations:
- Patient Instructions: Instruct patients to swallow tablets whole unless otherwise directed. Chewable tablets should be chewed thoroughly.
- Food and Drink: Some tablets should be taken with food to enhance absorption or reduce GI irritation.
iii. Dissolution and Absorption:
- Bioavailability: The extent and rate at which the active ingredient or active moiety is absorbed and becomes available at the site of action.
- First-Pass Effect: Drugs absorbed through the GI tract are subjected to first-pass metabolism in the liver, which may reduce the drug’s efficacy.
b. Capsules

i. Types of Capsules:
- Hard Capsules: These consist of two interlocking halves and are commonly used for powdered or granulated medications.
- Soft Gelatin Capsules: Used for liquid medications or oil-based solutions.
ii. Administration Considerations:
- Swallowing: Capsules should be swallowed whole. Some capsules are designed to be opened, but this should only be done if instructed by a healthcare provider.
- Special Formulations: Extended-release or enteric-coated capsules should not be crushed or chewed as it may alter the medication’s effect.
iii. Dissolution and Absorption:
- Gastric Emptying: Capsules generally dissolve in the stomach or small intestine, where the drug is absorbed.
c. Liquids
i. Types of Liquid Medications:
- Solutions: Medications are dissolved in a solvent (e.g., water or syrup).
- Suspensions: Solid particles are suspended in a liquid medium and must be shaken before administration.
- Emulsions: A mixture of oil and water with medications dispersed throughout.
ii. Administration Considerations:
- Measuring: Use appropriate measuring devices (e.g., oral syringes, measuring cups) to ensure accurate dosing.
- Storage: Some liquid medications require refrigeration or protection from light.
iii. Absorption and Onset:
- Rapid Absorption: Liquids are generally absorbed more quickly than tablets or capsules due to their form, which allows faster dissolution.
2. Topical Administration
Topical administration involves applying medication directly to the skin or mucous membranes. This route is used for both localized and systemic effects.
a) Creams

i. Characteristics:
- Composition: Creams are emulsions of oil and water, providing a moisturizing effect.
- Absorption: They are absorbed into the skin but may also leave a residue.
ii. Administration Considerations:
- Application: Apply a thin layer to the affected area and rub in gently.
- Hygiene: Wash hands before and after application to prevent contamination.
iii. Indications:
- Skin Conditions: Used for conditions such as eczema, psoriasis, and fungal infections.
b) Ointments

i. Characteristics:
- Composition: Ointments are oil-based, providing a barrier to moisture loss and a longer-lasting effect compared to creams.
- Absorption: They are less absorbed into the skin compared to creams but provide a more prolonged effect.
ii. Administration Considerations:
- Application: Apply to the affected area in a thin layer and cover if necessary.
- Potential for Occlusion: Ointments may trap heat and moisture, which can be beneficial or detrimental depending on the condition.
iii. Indications:
- Dry Skin Conditions: Often used for chronic skin conditions where a moisture barrier is required.
c. Patches

i. Characteristics:
- Design: Patches deliver medication through the skin over an extended period.
- Mechanism: Patches use a controlled release system to deliver medication continuously.
ii. Administration Considerations:
- Application Site: Apply to clean, dry skin. Rotate application sites to avoid skin irritation.
- Duration: Follow specific instructions regarding how long to wear the patch.
iii. Indications:
- Chronic Pain: Often used for pain management (e.g., fentanyl patches).
- Hormonal Replacement: Used for hormone therapy (e.g., estrogen patches).
3. Parenteral Administration
Parenteral administration involves injecting medication directly into the body, bypassing the GI tract. It is used when oral administration is not feasible or when a rapid onset of action is required.
a) Intramuscular (IM) Injection

i. Sites:
- Deltoid: Located in the upper arm; commonly used for vaccines.
- Vastus Lateralis: Located in the thigh; used for larger volumes and infants.
- Gluteal: Located in the buttock; used for larger volumes and certain medications.
ii. Techniques:
- Aseptic Technique: Ensure proper sterilization of the site and equipment to prevent infection.
- Needle Selection: Use appropriate needle length and gauge based on the injection site and medication type.
- Injection Angle: Insert the needle at a 90-degree angle to the skin.
iii. Considerations:
- Absorption Rate: IM injections are absorbed more rapidly than subcutaneous injections but slower than intravenous administration.
- Volume Limit: Typically, a maximum of 3 mL can be administered per site.
b) Intravenous (IV) Injection

i. Methods:
- Direct Injection (Bolus): A single, concentrated dose administered rapidly into the vein.
- Infusion: Medication delivered continuously or intermittently over time.
ii. Infusion Pumps:
- Types: Volumetric pumps, syringe pumps, and patient-controlled analgesia (PCA) pumps.
- Functions: Pumps regulate the flow rate and volume of medication, ensuring accurate delivery.
- Maintenance: Regularly check the pump settings and infusion site for complications such as infiltration or phlebitis.
iii. Considerations:
- Onset of Action: IV administration provides immediate therapeutic effects.
- Complications: Risks include infection, thrombosis, and extravasation.
c. Subcutaneous (SC) Injection

i. Sites:
- Abdomen: Preferred site for insulin administration.
- Thigh: Common for vaccinations and other medications.
- Upper Arm: Used for various medications, including some biologics.
ii. Techniques:
- Aseptic Technique: Ensure cleanliness of the site and equipment.
- Needle Selection: Use shorter needles compared to IM injections; typically 25-27 gauge.
- Injection Angle: Insert the needle at a 45 to 90-degree angle depending on the amount of subcutaneous tissue.
iii. Considerations:
- Volume Limit: Typically, a maximum of 1 mL is administered per site.
- Absorption Rate: SC injections are absorbed more slowly compared to IM injections but faster than oral medications.
4. Inhalational Administration

Inhalational administration involves delivering medication directly to the respiratory tract. This route is used for respiratory conditions and provides a localized effect with minimal systemic side effects.
a) Metered-Dose Inhalers (MDIs)
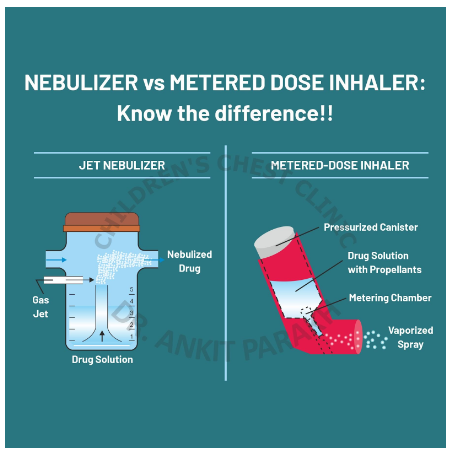
i. Characteristics:
- Design: MDIs use a pressurized canister to deliver a specific dose of medication in aerosol form.
- Activation: Inhalers require coordination between inhalation and actuation.
ii. Administration Techniques:
- Preparation: Shake the inhaler and attach the spacer if used.
- Inhalation: Breathe in deeply and slowly while pressing the canister to ensure medication reaches the lungs.
- Post-Inhalation: Rinse the mouth to reduce the risk of oral thrush with corticosteroid inhalers.
iii. Considerations:
- Technique: Proper technique is essential for effective medication delivery.
- Maintenance: Regular cleaning of the inhaler is necessary to prevent blockages.
b) Nebulizers

i. Characteristics:
- Design: Nebulizers convert liquid medication into a fine mist that is inhaled through a mask or mouthpiece.
- Types: Jet nebulizers and ultrasonic nebulizers.
ii. Administration Techniques:
- Preparation: Assemble the nebulizer according to the manufacturer’s instructions and add the prescribed medication.
- Inhalation: Breathe normally through the mouthpiece or mask until the medication is fully nebulized.
- Post-Inhalation: Clean the nebulizer components thoroughly after each use.
iii. Considerations:
- Duration: Nebulization typically takes 10-15 minutes.
- Maintenance: Regular cleaning and replacement of parts are necessary to ensure proper function and hygiene.
Safety and Accuracy
Ensuring safety and accuracy in medication administration is paramount to effective patient care. This section provides an extensive overview of the Five Rights of Medication Administration and Double-Check Procedures, crucial elements in preventing medication errors and ensuring optimal therapeutic outcomes.
1. Five Rights of Medication Administration
The Five Rights of Medication Administration are fundamental principles that guide the safe and accurate delivery of medications. Adhering to these rights helps prevent errors and enhances patient safety.
a) Right Patient
i. Identification Techniques:
- Use of Identification Bands: Verify patient identity using wristbands or other identification methods. Ensure the band is current and matches the patient’s medical records.
- Patient Confirmation: Ask the patient to state their full name and date of birth. This method is effective but should be complemented with other verification techniques.
ii. Verification Procedures:
- Cross-Checking with Records: Compare patient details on the medication order with those in the electronic health record (EHR) or paper chart.
- Patient Identification Systems: Use barcoding or RFID systems where available to match the medication with the patient’s record accurately.
iii. Challenges and Solutions:
- Patient Confusion: Some patients may have cognitive impairments or language barriers. Use clear, respectful communication and verify identity multiple ways.
- Multiple Patients with Similar Names: Implement additional checks, such as confirming patient identifiers beyond just name and date of birth.
b) Right Drug
i. Verification Process:
- Drug Label Review:

Check the medication label against the medication order or electronic prescription. Ensure that the drug name, dosage, and formulation match the order.
- Drug Storage: Ensure that the medication is stored correctly and is not expired. Check for any potential mix-ups in the medication storage area.
ii. Drug Administration Systems:
- Automated Dispensing Systems: Use automated systems for dispensing and checking medications to reduce human error.
- Electronic Medication Administration Records (eMAR): Use eMAR systems to track and verify medications administered.
iii. Challenges and Solutions:
- Look-Alike, Sound-Alike Drugs: Be aware of medications with similar names and verify each drug carefully. Utilize tall-man lettering to differentiate these medications.
- Unclear Prescriptions: Clarify any ambiguous drug orders with the prescribing provider before administration.
c) Right Dose
i. Calculation Techniques:
- Dose Calculations: Perform dose calculations based on the medication order. Use appropriate formulas and units to ensure accuracy.
- Conversion Calculations: Convert units correctly if required, such as converting milligrams to grams or milliliters to liters.
ii. Measurement Tools:
- Use of Appropriate Devices: Use calibrated devices like syringes, dropper, or measuring cups for accurate measurement of medication doses.
- Double-Check Dosages: Always verify dosages with another healthcare professional if required by protocol.
iii. Challenges and Solutions:
- Dosing Errors: Be vigilant about potential errors in dose calculation or measurement. Double-check calculations and measurements, especially with high-risk medications.
- Pediatric and Geriatric Doses: Adjust doses based on patient age, weight, and clinical condition. Use weight-based dosing calculators when necessary.
d) Right Route
i. Route Verification:
- Confirm Administration Route: Ensure the medication is administered via the prescribed route (oral, IV, IM, SC, etc.) as specified in the order.
- Assess Route-Specific Techniques: Use proper techniques for each route to maximize efficacy and minimize complications.
ii. Route-Specific Considerations:
- Oral Route: Ensure the patient can swallow tablets or capsules and understand how to take liquid medications.
- Parenteral Routes: Follow aseptic techniques for injections and verify injection sites.
iii. Challenges and Solutions:
- Route Confusion: Double-check the route specified in the medication order to avoid administering a drug via the wrong route.
- Patient Conditions: Adapt administration techniques based on patient conditions, such as avoiding oral medications in patients with swallowing difficulties.
e. Right Time
i. Timing Protocols:
- Scheduled Times: Administer medications at the prescribed times. Follow specific protocols for medications requiring timing precision, such as antibiotics or anticoagulants.
- Time Intervals: Adhere to time intervals between doses as specified in the medication order.
ii. Administration Scheduling:
- Medication Administration Record (MAR): Use MARs to track medication timing and ensure timely administration.
- Adjustments for Special Conditions: Make adjustments for special conditions like fasting or meal times, and document any changes in timing.
iii. Challenges and Solutions:
- Missed Doses: Implement strategies to avoid missed doses, such as using reminders or electronic alerts.
- Timing Errors: Verify timing protocols and make sure to account for time zone differences or shift changes if relevant.
2. Double-Check Procedures
Double-check procedures are critical for preventing medication errors and ensuring patient safety. Implementing thorough verification processes helps identify and correct potential mistakes before they reach the patient.
a) Verification Processes
i. Two-Person Verification:
- Collaborative Checks: Implement a two-person verification process for high-risk medications or complex doses. Both individuals should independently verify the medication, dose, and patient information.
- Cross-Checking: Use a standardized checklist to ensure all aspects of the medication order and administration are reviewed.
ii. Electronic Verification Systems:
- Barcoding Systems: Utilize barcoding systems to scan and verify medication and patient information electronically, reducing human error.
- Integrated Systems: Use integrated EHR and eMAR systems to cross-check medication orders and administration records.
iii. Documentation:
- Record Keeping: Document all verification steps, including any discrepancies and corrective actions taken.
- Audit Trails: Maintain audit trails for medication administration to track and review any errors or issues.
b. Error Prevention Strategies
i. Education and Training:
- Regular Training: Provide ongoing education and training for healthcare staff on medication administration protocols and error prevention strategies.
- Simulation Exercises: Use simulation exercises to practice and reinforce proper medication administration techniques.
ii. Standard Operating Procedures (SOPs):
- Develop SOPs: Establish and regularly update SOPs for medication administration and double-check procedures.
- Compliance Monitoring: Monitor compliance with SOPs and address any deviations or issues promptly.
iii. Reporting and Learning:
- Error Reporting Systems: Implement a non-punitive error reporting system to encourage staff to report medication errors or near misses.
- Root Cause Analysis: Conduct root cause analyses for reported errors to identify underlying issues and implement corrective actions.
c. ase Studies and Examples
i. High-Profile Medication Errors:
- Case Study Analysis: Review case studies of high-profile medication errors to understand common pitfalls and prevention strategies.
- Learning from Mistakes: Use these case studies as educational tools to highlight the importance of adherence to the Five Rights and double-check procedures.
ii. Simulation Scenarios:
- Real-Life Scenarios: Create simulation scenarios that replicate potential medication errors and practice double-check procedures.
- Feedback and Improvement: Provide feedback and identify areas for improvement based on simulation exercises.
