Side Effects and Adverse Reactions
Side Effects and Adverse Reactions
1. Side Effects
Common Side Effects
1.1 Nausea

Pathophysiology and Mechanisms: Nausea is a subjective sensation characterized by an unpleasant feeling that often precedes vomiting. It results from the stimulation of the central nervous system, specifically the vomiting center in the medulla oblongata. Various neurotransmitters, such as serotonin, dopamine, and histamine, play crucial roles in this process. The chemoreceptor trigger zone (CTZ), located in the area postrema of the brain, is also involved in detecting toxins and inducing nausea.
Common Causes of Nausea Related to Medications:
- Opioids: These drugs, used for pain management, can stimulate the CTZ, leading to nausea and vomiting. They may also affect gastrointestinal motility, contributing to the sensation of nausea.
- Antibiotics: Some antibiotics, such as erythromycin, can cause gastrointestinal upset and nausea due to their direct irritant effects on the stomach lining.
- Chemotherapy Agents: Drugs used in cancer treatment, such as cisplatin and cyclophosphamide, induce nausea through their emetogenic properties, affecting the gastrointestinal tract and central nervous system.
Management and Nursing Considerations:
- Antiemetic Medications: Drugs like ondansetron (a 5-HT3 receptor antagonist) and metoclopramide (a dopamine antagonist) can be administered to alleviate nausea.
- Patient Education: Educate patients on the importance of taking medications with food to minimize gastrointestinal irritation and to report severe or persistent nausea.
1.2 Headache
Pathophysiology and Mechanisms: Headaches can be a result of various mechanisms including vasodilation, increased intracranial pressure, and muscle tension. Medications can induce headaches through different pathways such as altering cerebral blood flow or irritating cranial nerves.
Common Causes of Headaches Related to Medications:
- Vasodilators:

Drugs like nitrates and calcium channel blockers, used for hypertension and angina, can cause headaches due to their vasodilatory effects.
- Hormonal Contraceptives: Estrogen-containing contraceptives can cause headaches due to hormonal fluctuations and changes in blood flow.
Management and Nursing Considerations:
- Analgesics: Nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen can be used to manage medication-induced headaches.
- Monitoring: Regular monitoring of headache patterns and intensities to differentiate between medication-related headaches and other types of headaches.
1.3 Dizziness

Pathophysiology and Mechanisms: Dizziness can be caused by a variety of factors including hypotension, vestibular disturbances, or changes in cerebral blood flow. Medications that affect blood pressure or the central nervous system can contribute to dizziness.
Common Causes of Dizziness Related to Medications:
- Antihypertensives: Drugs like beta-blockers and diuretics can cause dizziness by lowering blood pressure and affecting cerebral perfusion.
- Sedatives and Hypnotics: Medications such as benzodiazepines and barbiturates can cause dizziness due to their central nervous system depressant effects.
Management and Nursing Considerations:
- Dose Adjustment: Adjusting the dosage of the offending medication may help alleviate dizziness.
- Safety Measures: Advise patients to rise slowly from sitting or lying positions to prevent orthostatic hypotension and resultant dizziness.
1.4 Drowsiness

Pathophysiology and Mechanisms: Drowsiness is characterized by a reduced level of consciousness and impaired alertness. It can be induced by medications that depress the central nervous system or alter neurotransmitter levels involved in wakefulness.
Common Causes of Drowsiness Related to Medications:
- Antihistamines: First-generation antihistamines such as diphenhydramine can cause drowsiness due to their central anticholinergic effects.
- Antidepressants: Tricyclic antidepressants like amitriptyline can cause sedation as a side effect due to their antihistaminic and anticholinergic properties.
Management and Nursing Considerations:
- Alternative Medications: Consider prescribing non-sedating alternatives for patients who need to avoid drowsiness.
- Patient Education: Educate patients on the potential impact of drowsiness on activities such as driving and operating machinery.
Drug-Specific Side Effects
2.1 Antihistamines
Mechanism of Action: Antihistamines block histamine H1 receptors, which are responsible for allergic reactions. First-generation antihistamines, such as diphenhydramine, can cross the blood-brain barrier and affect the central nervous system, leading to sedation.
Drug-Specific Side Effects:
- Sedation: First-generation antihistamines can cause significant drowsiness due to their central action.
- Anticholinergic Effects: These include dry mouth, blurred vision, and constipation.
Management and Nursing Considerations:
- Alternatives: Use second-generation antihistamines like loratadine or cetirizine, which are less likely to cause sedation.
- Patient Monitoring: Monitor for signs of anticholinergic effects and educate patients on managing these symptoms.
2.2 Opioids
Mechanism of Action: Opioids bind to opioid receptors in the central nervous system, leading to pain relief. They also affect other systems, causing side effects such as nausea and constipation.
Drug-Specific Side Effects:
- Constipation: Opioids decrease gastrointestinal motility, leading to constipation.
- Respiratory Depression: High doses can suppress the respiratory drive, leading to potential respiratory complications.
Management and Nursing Considerations:
- Laxatives: Prescribe stool softeners or laxatives to manage opioid-induced constipation.
- Monitoring: Regularly monitor respiratory rate and assess for signs of opioid overdose.
2.3 Antibiotics
Mechanism of Action: Antibiotics work by targeting specific bacterial processes, but they can also affect normal flora and gastrointestinal mucosa.
Drug-Specific Side Effects:
- Gastrointestinal Upset: Nausea, vomiting, and diarrhea are common side effects due to the disruption of normal gut flora.
- Allergic Reactions: Some antibiotics, such as penicillin, can cause allergic reactions ranging from rash to anaphylaxis.
Management and Nursing Considerations:
- Probiotics: Consider recommending probiotics to reduce gastrointestinal disturbances.
- Allergy Monitoring: Monitor for signs of allergic reactions and educate patients to report any symptoms immediately.
2.4 Chemotherapy Agents
Mechanism of Action: Chemotherapy drugs target rapidly dividing cancer cells, but they can also affect normal, rapidly dividing cells, leading to side effects.
Drug-Specific Side Effects:
- Nausea and Vomiting: Common due to the emetogenic properties of many chemotherapy agents.
- Myelosuppression: Reduction in blood cell counts, leading to increased risk of infections and bleeding.
Management and Nursing Considerations:
- Anti-emetics: Administer anti-emetic drugs such as ondansetron or dexamethasone to manage nausea and vomiting.
- Blood Monitoring: Regularly monitor blood cell counts and provide supportive care as needed.
2.5 Antidepressants
Mechanism of Action: Antidepressants affect neurotransmitter levels in the brain, including serotonin and norepinephrine.
Drug-Specific Side Effects:
- Sexual Dysfunction: SSRIs and SNRIs can cause sexual side effects, including decreased libido and delayed orgasm.
- Weight Gain: Some antidepressants, such as tricyclics, can lead to significant weight gain.
Management and Nursing Considerations:
- Alternative Therapies: Consider alternative antidepressants with fewer sexual side effects if necessary.
- Patient Counseling: Discuss potential weight gain with patients and provide dietary and exercise recommendations.
Conclusion
In-depth understanding of side effects and adverse reactions to medications is essential for effective nursing care. By recognizing common side effects like nausea, headache, dizziness, and drowsiness, as well as drug-specific effects across various classes of medications, nurses can better manage patient outcomes. Proper management strategies, including the use of alternative medications, patient education, and regular monitoring, are crucial for minimizing adverse effects and ensuring patient safety.
Adverse Reactions
1.1 Allergic Reactions
1.1.1 Rashes

Pathophysiology and Mechanisms: Allergic rashes are a common type of adverse reaction and result from an immunologic response to a drug. The drug acts as an antigen, triggering the immune system to release histamines and other inflammatory mediators. This reaction leads to inflammation and irritation of the skin, manifesting as rashes.
Types of Rashes:
- Urticaria (Hives): Characterized by raised, itchy welts on the skin. It often results from the release of histamines.
- Erythema Multiforme: Presents as red patches or spots, sometimes with a target-like appearance. It may be associated with a drug-induced hypersensitivity reaction.
- Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN): Severe forms of drug-induced rashes characterized by extensive skin peeling and mucosal involvement. They are life-threatening and require immediate medical attention.
Common Drug-Induced Rashes:
- Antibiotics: Penicillins and sulfonamides are well-known for causing rashes.
- Anticonvulsants: Drugs like phenytoin and carbamazepine can induce rash as part of their hypersensitivity reactions.
- Allopurinol: Used for gout management, it can cause severe skin reactions including SJS and TEN.
Management and Nursing Considerations:
- Discontinuation of the Drug: Immediate cessation of the offending drug is crucial.
- Antihistamines and Corticosteroids: These may be used to manage mild to moderate rashes.
- Monitoring: Regularly monitor for signs of severe reactions and refer to a specialist if necessary.
1.1.2 Anaphylaxis

Pathophysiology and Mechanisms: Anaphylaxis is a severe, life-threatening allergic reaction that occurs rapidly after exposure to an allergen. It involves the systemic release of histamines and other mediators, causing vasodilation, increased vascular permeability, and bronchoconstriction.
Clinical Manifestations:
- Cutaneous Symptoms: Itching, hives, and swelling.
- Respiratory Symptoms: Dyspnea, wheezing, and stridor due to airway constriction.
- Cardiovascular Symptoms: Hypotension, tachycardia, and potential shock.
- Gastrointestinal Symptoms: Abdominal cramping, nausea, and vomiting.
Common Triggers of Anaphylaxis:
- Antibiotics: Particularly penicillin and other beta-lactams.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Such as ibuprofen and aspirin.
- Contrast Media: Used in radiological procedures.
Management and Nursing Considerations:
- Immediate Intervention: Administer epinephrine intramuscularly (typically in the mid-anterolateral thigh) and seek emergency medical help.
- Supportive Measures: Provide oxygen, intravenous fluids, and corticosteroids as necessary.
- Monitoring: Continuous monitoring of vital signs and response to treatment is essential.
1.2 Serious Reactions
1.2.1 Liver Toxicity
Pathophysiology and Mechanisms: Liver toxicity can result from drug-induced liver injury (DILI), where drugs cause damage to liver cells through various mechanisms such as oxidative stress, mitochondrial injury, or immune-mediated damage. The liver metabolizes many drugs, and its dysfunction can lead to severe systemic effects.
Common Drug-Induced Liver Toxicity:
- Acetaminophen: Overdose or chronic high doses can lead to acute liver failure.
- Antitubercular Drugs: Such as isoniazid and rifampin, known for causing hepatotoxicity.
- Methotrexate: Used in cancer and autoimmune diseases, can cause liver fibrosis and cirrhosis with prolonged use.
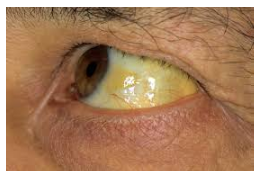
Clinical Manifestations:
- Jaundice: Yellowing of the skin and sclera due to elevated bilirubin levels.
- Elevated Liver Enzymes: Increased levels of alanine transaminase (ALT) and aspartate transaminase (AST).
- Abdominal Pain and Swelling: Indicative of liver inflammation or hepatomegaly.
Management and Nursing Considerations:
- Monitoring Liver Function Tests: Regular monitoring of liver enzymes and bilirubin levels.
- Drug Adjustment or Discontinuation: Altering the dosage or discontinuing the offending drug is often necessary.
- Supportive Care: Providing symptomatic relief and supportive care, including hydration and nutritional support.
1.2.2 Renal Impairment

Pathophysiology and Mechanisms: Renal impairment due to drugs can occur through direct nephrotoxicity or indirect effects. Drugs may cause damage to the kidneys’ glomeruli, tubules, or interstitium, leading to impaired renal function.
Common Drug-Induced Renal Impairment:
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Can cause acute kidney injury by reducing renal blood flow.
- Antibiotics: Such as aminoglycosides, can lead to nephrotoxicity.
- Angiotensin-Converting Enzyme (ACE) Inhibitors: May cause hyperkalemia and acute renal failure in susceptible individuals.
Clinical Manifestations:
- Elevated Serum Creatinine and Urea: Indicative of reduced kidney function.
- Edema: Fluid retention due to impaired renal filtration.
- Electrolyte Imbalances: Hyperkalemia and hyponatremia are common with renal impairment.
Management and Nursing Considerations:
- Monitoring Renal Function: Regular monitoring of serum creatinine, urea, and electrolytes.
- Dose Adjustments: Adjusting doses of nephrotoxic drugs or switching to alternatives with less renal impact.
- Hydration and Support: Ensuring adequate hydration and supportive care to mitigate renal stress.
1.2.3 Cardiac Events
Pathophysiology and Mechanisms: Drug-induced cardiac events can range from arrhythmias to ischemic heart disease. Medications may affect cardiac function by altering electrolyte balance, interfering with cardiac conduction, or causing vasoconstriction.
Common Drug-Induced Cardiac Events:
- QT Interval Prolongation:
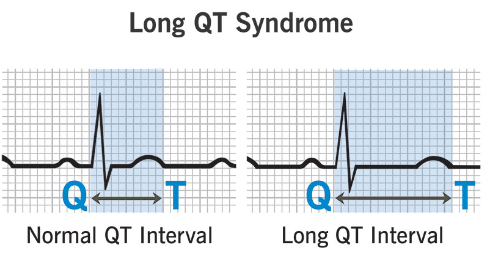
Drugs like certain antipsychotics and antibiotics can prolong the QT interval, leading to torsades de pointes (a type of life-threatening arrhythmia).
- Myocardial Infarction:
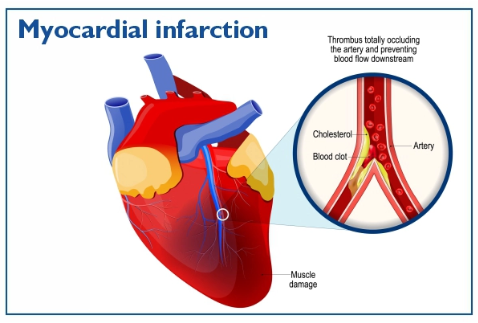
Some drugs, particularly those affecting lipid profiles, can increase the risk of myocardial infarction.
Clinical Manifestations:
- Arrhythmias: Palpitations, dizziness, or syncope due to irregular heartbeats.
- Chest Pain: Associated with myocardial infarction or angina.
- Heart Failure Symptoms: Such as shortness of breath, fatigue, and edema.
Management and Nursing Considerations:
- Electrocardiogram (ECG) Monitoring: Regular ECG monitoring to detect arrhythmias or QT prolongation.
- Medication Review: Reviewing and adjusting medications that may contribute to cardiac events.
- Emergency Intervention: Immediate treatment for severe cardiac events, including anti-arrhythmic drugs or emergency cardiology consultation.
1.3 Black Box Warnings
Definition and Purpose: Black Box Warnings are the most stringent warnings issued by the U.S. Food and Drug Administration (FDA) for drugs. They are used to highlight serious or life-threatening risks associated with the use of a medication. These warnings are typically included in the prescribing information and are intended to ensure that healthcare providers are aware of the potential risks and can make informed decisions.
Examples of Drugs with Black Box Warnings:
1.3.1 Antidepressants
Black Box Warning: Increased risk of suicidal thoughts and behaviors in children, adolescents, and young adults. This risk is particularly pronounced during the initial treatment period.
Clinical Considerations:
- Monitoring: Close monitoring of patients for any signs of worsening depression or emerging suicidal thoughts.
- Patient Education: Inform patients and caregivers about the potential risks and the importance of reporting any changes in mood or behavior.
1.3.2 Antipsychotics
Black Box Warning: Increased risk of death in elderly patients with dementia-related psychosis. These drugs have also been associated with an increased risk of cerebrovascular events.
Clinical Considerations:
- Alternatives: Consider alternative treatments for elderly patients with dementia-related psychosis.
- Monitoring: Regularly assess for signs of cerebrovascular events and monitor overall health.
1.3.3 Opioids
Black Box Warning: Risk of addiction, abuse, and misuse, which can lead to overdose and death. Opioids also have a risk of life-threatening respiratory depression.
Clinical Considerations:
- Patient Assessment: Thorough assessment of the patient’s history and risk factors for addiction.
- Monitoring: Regular monitoring for signs of opioid misuse and respiratory depression.
1.3.4 Acetaminophen
Black Box Warning: Risk of severe liver injury when doses exceed the recommended limit, especially in the context of chronic alcohol use.
Clinical Considerations:
- Dosing: Strict adherence to dosing guidelines and monitoring for signs of liver dysfunction.
- Patient Education: Educate patients on the risks of exceeding the recommended dose and the importance of avoiding alcohol while taking acetaminophen.
Conclusion
Understanding adverse reactions and black box warnings is essential for safe and effective nursing care. By recognizing and managing allergic reactions, serious adverse effects, and drugs with significant risks, nurses can help prevent and mitigate these potentially severe outcomes. Regular monitoring, patient education, and prompt intervention are crucial components of comprehensive pharmacological management.
Monitoring and Management
1.1 Monitoring Parameters
1.1.1 Laboratory Tests
Laboratory tests are crucial for detecting and managing side effects and adverse reactions to medications. They provide objective data that can help guide treatment decisions, assess drug toxicity, and monitor the effectiveness of therapeutic interventions.
1.1.1.1 Complete Blood Count (CBC)
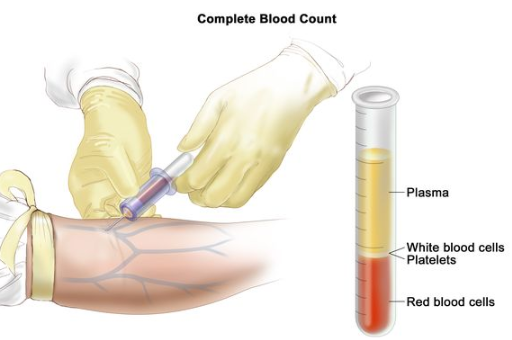
Purpose and Indications:
- Monitor for Hematologic Reactions: CBC is used to detect drug-induced hematologic abnormalities, such as anemia, leukopenia, thrombocytopenia, or leukocytosis.
- Drug Examples: Drugs like chemotherapy agents (e.g., cyclophosphamide), anticoagulants (e.g., heparin), and antiepileptics (e.g., carbamazepine) may affect blood cell counts.
Key Parameters:
- Hemoglobin and Hematocrit: Low levels may indicate anemia, often seen with drugs causing bone marrow suppression.
- White Blood Cell Count (WBC): Increased or decreased counts can signal infection, inflammation, or bone marrow suppression.
- Platelet Count: Essential for assessing bleeding risk or clotting disorders.
1.1.1.2 Liver Function Tests (LFTs)
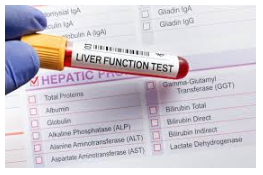
Purpose and Indications:
- Detect Hepatotoxicity: LFTs evaluate the impact of drugs on liver function, identifying potential liver damage or inflammation.
- Drug Examples: Acetaminophen, statins, and certain antibiotics are known for causing liver-related issues.
Key Parameters:
- Alanine Aminotransferase (ALT) and Aspartate Aminotransferase (AST): Elevated levels can indicate liver cell injury or inflammation.
- Alkaline Phosphatase (ALP) and Gamma-Glutamyl Transferase (GGT): Increased levels may suggest cholestasis or bile duct obstruction.
- Bilirubin: Elevated levels can signal liver dysfunction or hemolysis.
1.1.1.3 Renal Function Tests
Purpose and Indications:
- Assess Renal Impairment: Renal function tests monitor the kidneys’ ability to filter and excrete drugs, especially important for medications with known nephrotoxicity.
- Drug Examples: NSAIDs, ACE inhibitors, and certain antibiotics.
Key Parameters:
- Serum Creatinine: Elevated levels suggest impaired kidney function or acute kidney injury.
- Blood Urea Nitrogen (BUN): High levels can indicate renal dysfunction or dehydration.
- Electrolytes: Sodium, potassium, and other electrolytes are monitored for imbalances.
1.1.1.4 Electrolyte Panels
Purpose and Indications:
- Monitor Electrolyte Imbalances: Many drugs affect electrolyte levels, leading to conditions like hyperkalemia, hypokalemia, or hyponatremia.
- Drug Examples: Diuretics, corticosteroids, and some antipsychotics.
Key Parameters:
- Sodium and Potassium Levels: Imbalances can have significant cardiovascular and neurological effects.
- Calcium and Magnesium: Imbalances can affect neuromuscular function and cardiac rhythm.
1.1.1.5 Coagulation Tests
Purpose and Indications:
- Evaluate Bleeding Risks: Coagulation tests are vital for monitoring patients on anticoagulants or antiplatelet therapy.
- Drug Examples: Warfarin, heparin, and clopidogrel.
Key Parameters:
- Prothrombin Time (PT) and International Normalized Ratio (INR): Important for monitoring patients on warfarin.
- Activated Partial Thromboplastin Time (aPTT): Used for monitoring heparin therapy.
- Platelet Count: Assesses bleeding risk and platelet function.
1.1.2 Vital Signs
Vital signs are essential indicators of a patient’s overall health and can provide early warnings of adverse drug reactions.
1.1.2.1 Blood Pressure
Purpose and Indications:
- Detect Hypertension or Hypotension: Blood pressure monitoring is crucial for drugs affecting cardiovascular function.
- Drug Examples: Antihypertensives, diuretics, and vasopressors.
Key Parameters:
- Systolic and Diastolic Pressure: Regular monitoring helps prevent or manage drug-induced hypertension or hypotension.
- Orthostatic Changes: Assess for postural hypotension, especially with medications affecting fluid balance or vascular tone.
1.1.2.2 Heart Rate
Purpose and Indications:
- Monitor for Arrhythmias: Changes in heart rate can indicate drug-induced cardiac effects.
- Drug Examples: Antiarrhythmics, beta-blockers, and certain antidepressants.
Key Parameters:
- Resting Heart Rate: Regular monitoring for bradycardia or tachycardia.
- Rhythm Assessment: Detect arrhythmias through electrocardiogram (ECG) if necessary.
1.1.2.3 Respiratory Rate
Purpose and Indications:
- Assess Respiratory Function: Vital for detecting drug-induced respiratory depression or distress.
- Drug Examples: Opioids, sedatives, and anesthetics.
Key Parameters:
- Respiratory Rate: Monitor for signs of hypoventilation or tachypnea.
- Oxygen Saturation: Assess with pulse oximetry, especially in patients on respiratory depressants.
1.1.2.4 Temperature
Purpose and Indications:
- Monitor for Fever or Hypothermia: Temperature changes can indicate infections or drug reactions.
- Drug Examples: Antibiotics, antipyretics, and certain chemotherapeutic agents.
Key Parameters:
- Body Temperature: Regular monitoring to detect fever or hypothermia.
- Fever Patterns: Document and evaluate fever patterns in relation to drug administration.
1.2 Reporting and Documentation
1.2.1 Reporting Adverse Effects to Appropriate Agencies
Purpose and Importance:
- Ensure Patient Safety: Reporting adverse effects helps identify potential safety concerns and contributes to public health surveillance.
- Facilitate Drug Monitoring: Helps regulatory agencies monitor the safety profile of medications and make informed decisions about drug use.
1.2.1.1 Methods of Reporting
Internal Reporting:
- Institutional Protocols: Follow hospital or clinic protocols for reporting adverse drug reactions (ADRs) to the pharmacy and therapeutics committee or adverse events reporting system.
- Electronic Health Records (EHRs): Document adverse effects in patient records, ensuring accurate and complete information.
External Reporting:
- Food and Drug Administration (FDA): In the U.S., report to the FDA’s MedWatch program for serious adverse events.
- Other Regulatory Agencies: Report to agencies like the European Medicines Agency (EMA) or Health Canada, depending on the region.
1.2.1.2 Documentation Requirements
Essential Information:
- Patient Information: Include patient demographics, medical history, and current medications.
- Drug Details: Document the drug name, dosage, route, and duration of use.
- Adverse Effect Description: Provide a detailed description of the adverse effect, including onset, severity, and any intervention required.
- Outcome: Note the patient’s response to treatment and any changes in their condition.
1.2.1.3 Follow-Up Actions
Monitor for Recurrence:
- Ongoing Assessment: Continue to monitor the patient for any recurrence of the adverse effect or new symptoms.
- Adjustments: Make necessary adjustments to the patient’s medication regimen based on the adverse reaction and follow-up evaluations.
1.2.2 Documentation in the Medical Record
Importance and Guidelines:
- Accuracy: Ensure that all relevant details about the adverse effect are documented accurately and promptly.
- Consistency: Use standardized terminology and formats to maintain consistency across medical records.
Components of Documentation:
- Patient Identification: Ensure correct patient identification details.
- Date and Time: Record the date and time of the adverse effect and any interventions.
- Clinical Assessment: Document the clinical findings, diagnostic tests, and treatments administered.
- Patient Communication: Note any discussions with the patient or their family regarding the adverse effect and subsequent management.
Best Practices for Documentation:
- Timeliness: Document adverse effects as soon as they are identified to ensure accurate and up-to-date records.
- Detail: Include comprehensive details to facilitate accurate analysis and follow-up.
- Legal and Ethical Considerations: Ensure that documentation meets legal and ethical standards, including patient confidentiality and informed consent.
Conclusion
Effective monitoring and management of side effects and adverse reactions are critical for ensuring patient safety and optimizing therapeutic outcomes. By systematically utilizing laboratory tests and vital signs, and adhering to rigorous reporting and documentation practices, healthcare professionals can enhance their ability to detect, manage, and mitigate adverse drug reactions. This comprehensive approach helps in maintaining high standards of patient care and contributes to the broader goal of improving medication safety and efficacy.
