Mobility/Immobility
-
Identify Signs and Symptoms of Venous Insufficiency and Intervene to Promote Venous Return (e.g., Elastic Stockings, Sequential Compression Device)
Venous Insufficiency Overview

Venous insufficiency occurs when the veins in the legs are unable to efficiently return blood to the heart, often resulting in blood pooling in the lower extremities. This condition is common in patients with varicose veins, deep vein thrombosis (DVT), obesity, and those with a sedentary lifestyle or prolonged standing.
Signs and Symptoms of Venous Insufficiency
- Edema: Swelling of the legs, especially in the lower extremities, is a hallmark symptom. This can be particularly noticeable by the end of the day.
- Pain and Discomfort: Patients often experience a heavy or aching sensation in the legs, which can worsen with prolonged standing or sitting.
- Skin Changes: The skin may become discolored (brownish tint), thin, and fragile. Stasis dermatitis or ulcers may develop over time.
- Varicose Veins: Enlarged, twisted veins, which are visible under the skin, often accompany venous insufficiency.
- Phlebitis: Inflammation of the veins, which may be associated with pain, warmth, and redness along the affected vein.
- Leg Cramps and Restlessness: Patients may complain of leg cramps, particularly at night, and a sensation of restless legs due to poor circulation.
Interventions to Promote Venous Return
The goal of treatment for venous insufficiency is to improve circulation and reduce symptoms such as swelling and pain. Several nursing interventions can be used to promote venous return, which are essential for improving patient comfort and preventing complications like ulcers and venous stasis.
- Elastic Stockings (Compression Stockings):
- Purpose: Elastic stockings are designed to apply graduated compression to the legs, which helps to prevent the pooling of blood and promotes upward blood flow towards the heart.
- Mechanism: The stockings exert the most pressure at the ankle, decreasing progressively toward the thigh. This helps to move blood through the veins and prevents venous stasis.
- Application: Nurses should ensure that the stockings are put on in the morning, before swelling has occurred, to achieve the maximum benefit. They must be properly fitted to avoid discomfort and further issues.
- Nursing Considerations: Educating the patient on how to wear, care for, and clean the stockings is crucial. Nurses should inspect the patient’s skin regularly for any signs of irritation or skin breakdown.
- Sequential Compression Devices (SCDs):
- Purpose: SCDs are pneumatic devices that inflate and deflate in a sequential manner to mimic the natural contraction of leg muscles, promoting blood flow back to the heart and reducing the risk of DVT and venous insufficiency.
- Application: The device is typically used in hospitalized patients, particularly those on bed rest or recovering from surgery.
- Nursing Considerations: Nurses should monitor for proper placement, ensure that the device is functioning properly, and assess for any signs of discomfort or skin breakdown from the cuffs. Regular assessments for signs of DVT (such as swelling, pain, or redness) should be conducted.
- Elevation of the Legs:
- Purpose: Elevating the legs above the level of the heart helps facilitate venous return by using gravity to move blood back to the upper body.
- Application: Encourage patients to elevate their legs when resting, ideally for 15-30 minutes, several times a day.
- Nursing Considerations: Ensure that the patient is comfortable and that the legs are supported properly to avoid pressure ulcers or joint stiffness.
- Exercise:
- Purpose: Regular physical activity, especially walking, helps strengthen the calf muscles, which are key to pumping blood back to the heart.
- Nursing Considerations: Educating patients on the importance of regular walking and leg exercises (e.g., ankle pumps, toe raises) is essential for improving circulation.
- Weight Management:
- Purpose: Obesity is a significant risk factor for venous insufficiency. Reducing weight can decrease pressure on the veins and improve circulation.
- Nursing Considerations: Nurses can offer support in the form of diet education, referrals to nutritionists, and encouragement for gradual weight loss.
-
Check Client for Mobility, Gait, Strength, Motor Skills
Mobility Assessment
A thorough mobility assessment is necessary to evaluate a client’s ability to move and perform activities of daily living (ADLs). This includes an evaluation of the client’s gait, strength, and motor skills.
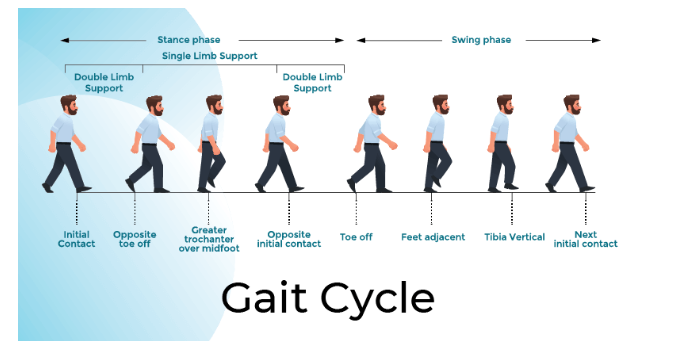
- Gait:
- Definition: Gait refers to the pattern or manner of walking. A change in gait can indicate various health problems, including musculoskeletal, neurological, or cardiovascular issues.
- Assessment: Observe the patient’s walking pattern for abnormalities such as limping, shuffling, or unsteady walking. Gait should be assessed both with and without assistive devices if applicable.
- Normal Gait: A normal gait is smooth, balanced, and coordinated, with a consistent rhythm and even stride length.
- Abnormal Gait: Abnormalities such as an unsteady gait, uneven steps, or dragging of the feet should be noted. This may indicate conditions like ataxia, Parkinson’s disease, or musculoskeletal impairments.
- Strength:
- Definition: Muscle strength is the ability to contract and exert force against resistance. A decrease in strength can affect the patient’s mobility and ability to perform ADLs.
- Assessment: Nurses assess muscle strength using a scale from 0 to 5:
- 0: No contraction
- 1: Flicker of contraction
- 2: Active movement without gravity
- 3: Active movement against gravity
- 4: Active movement against some resistance
- 5: Normal muscle strength
- Nursing Considerations: Regular strength assessments are essential for tracking changes in the patient’s condition, especially in those recovering from surgery, injury, or neurological conditions.
- Motor Skills:
- Definition: Motor skills refer to the ability to perform coordinated movements, including fine motor (e.g., grasping a pen) and gross motor (e.g., walking, sitting up).
- Assessment: Test fine motor skills by asking the patient to perform tasks like buttoning a shirt, picking up objects, or writing. Gross motor skills can be evaluated by observing the patient while they stand, walk, and sit.
- Nursing Considerations: Changes in motor skills may indicate neurological deficits, such as those caused by stroke, Parkinson’s disease, or spinal cord injury. Early identification of motor skill issues can help prevent complications like falls.
-
Provide for Mobility Needs (e.g., Ambulation, Range of Motion, Transfer, Repositioning, Use of Adaptive Equipment)
Ambulation

Ambulation refers to the ability to walk or move independently. In hospitalized or immobile patients, it is vital to maintain or improve mobility to prevent complications such as pneumonia, blood clots, and muscle atrophy.
- Nursing Interventions:
- Assistive Devices: Utilize devices like walkers, canes, or crutches to promote independence and reduce the risk of falls.
- Gradual Progression: When a patient is not able to ambulate independently, it is important to gradually increase the duration and distance they walk, starting with short walks and progressing as tolerated.
- Safety Measures: Ensure that the environment is free from obstacles and that the patient’s shoes are non-slip. Always monitor for signs of fatigue or instability.
Range of Motion (ROM)
ROM exercises are used to maintain or improve joint mobility, flexibility, and muscle strength. These exercises can be active or passive, depending on the patient’s level of mobility.
- Active ROM: The patient performs the exercises independently, moving their joints through their full range of motion.
- Passive ROM: The nurse or caregiver assists in moving the patient’s joints through their full range of motion when the patient is unable to do so independently.
- Nursing Considerations:
- Frequency: ROM exercises should be performed multiple times a day, especially in patients who are bedridden or have limited mobility.
- Pain Management: Monitor the patient for discomfort and modify the exercises as needed to prevent injury. It is essential to educate the patient on how to report pain during the exercises.
Transfer and Repositioning

Proper techniques for transferring and repositioning patients are critical for preventing falls, skin breakdown, and muscle strain.
- Transfer Techniques:
- Mechanical Lifts: For patients who are unable to transfer independently, a mechanical lift (e.g., Hoyer lift) should be used to ensure safety.
- Assistance from Caregivers: When lifting or transferring a patient manually, the nurse should ensure proper body mechanics to prevent injury. This includes bending at the knees, using leg muscles, and keeping the patient close to the body.
- Repositioning:
- Prevention of Pressure Ulcers: Repositioning patients regularly (every 2 hours in bed, every hour in a chair) helps to relieve pressure on bony prominences, preventing pressure ulcers.
- Technique: Ensure that patients are positioned with pillows to support proper alignment and comfort.
-
Reinforce Client Teaching on Methods to Maintain Mobility (e.g., Active/Passive ROM, Strengthening, Isometric Exercises)
Teaching Active and Passive Range of Motion (ROM) Exercises
Range of motion exercises are essential in maintaining or restoring joint movement and preventing contractures.
- Active ROM: Instruct the patient to move their joints independently through the full range of motion.
- Passive ROM: Teach caregivers or healthcare workers to gently move the patient’s joints through their full range of motion if the patient is unable to do so themselves.
Strengthening Exercises
Strengthening exercises focus on increasing muscle strength and endurance. These exercises can be beneficial for patients with musculoskeletal or neurological conditions.
- Isometric Exercises: Instruct patients on how to perform isometric exercises, where muscles are tensed without movement. These can be particularly useful for patients who are immobile or have limited strength.
- Progressive Resistance: Gradually increase the resistance or number of repetitions to improve muscle strength over time.
Nursing Considerations: Educate patients on the importance of consistency with exercises to see results. Reinforce proper techniques to prevent strain or injury.
-
Use Measures to Maintain or Improve Client Skin Integrity
Skin integrity is a critical aspect of patient care, especially in immobile clients. Measures to maintain healthy skin include:
- Hydration: Keep the skin hydrated to prevent dryness and cracking.
- Frequent Position Changes: Repositioning patients regularly can prevent pressure ulcers and skin breakdown.
- Use of Barrier Creams: Apply barrier creams to protect skin from moisture and prevent irritation.
-
Maintain Correct Client Body Alignment

Proper body alignment is essential for comfort, musculoskeletal health, and effective breathing. Ensuring that the client is positioned with the head, neck, and spine in a neutral position can reduce pressure on joints and muscles.
- Positioning Techniques: Use pillows or supports to maintain alignment and prevent contractures.
- Repositioning: Regular repositioning is necessary to maintain body alignment and prevent complications such as pressure ulcers.
-
Provide Care to an Immobilized Client Based on Need
Immobilized clients require specific care to maintain their physical and emotional well-being. Nursing interventions may include:
- Physical Therapy: Involvement of physical therapy to maintain or regain movement.
- Psychosocial Support: Address emotional well-being through communication, support, and activities that stimulate mental engagement.
- Pain Management: Carefully manage any pain related to immobility, including the use of medication and non-pharmacological strategies.
