Dosage Calculations
This chapter provides a comprehensive overview of dosage calculations, focusing on essential principles such as units of measurement, performing dosage calculations, and considerations for specific populations. Mastery of these concepts is critical for safe medication administration in nursing practice.
Calculating Dosages
Calculating dosages accurately is a fundamental skill for nurses, as medication errors can have serious implications for patient safety. This section will delve into the critical aspects of dosage calculations, including understanding units of measurement, performing various calculation methods, and addressing special considerations for pediatric and geriatric populations.
Units of Measurement
Understanding units of measurement is essential for effective dosage calculations. Medications can be measured using various systems, and familiarity with these units allows nurses to calculate dosages accurately and safely.
Understanding Metric Conversions
- Metric System Overview:
- The metric system is a decimal-based system of measurement widely used in healthcare. Key units in pharmacology include milligrams (mg), grams (g), liters (L), and milliliters (mL). Understanding the relationships between these units is vital for accurate dosing.
- Common Metric Units:
- Weight: 1 g = 1000 mg
- Volume: 1 L = 1000 mL
- Length: 1 m = 100 cm = 1000 mm
- Metric Conversions:
- Converting between units involves multiplication or division based on the metric relationships. For example:
- To convert milligrams to grams:
- Grams = milligrams * 1000
- Example: Convert 2500 mg to grams:
- 2500 mg ÷ 1000 = 2.5 g
- To convert liters to milliliters:
- milliliters=liters×1000\text{milliliters} = \text{liters} \times 1000 milliliters=liters×1000
- Example: Convert 3 L to mL:
- 3 L × 1000 = 3000 mL
- To convert milligrams to grams:
- Converting between units involves multiplication or division based on the metric relationships. For example:
- Importance of Accurate Conversions:
- Accurate metric conversions prevent medication errors and ensure patients receive the correct dosages. Nurses must double-check conversions, especially when working with high-alert medications.
Familiarity with Household Measurements
- Common Household Measurements:
- In addition to the metric system, nurses often encounter household measurements, particularly in pediatric dosing. Common units include:
- Teaspoon (tsp): 1 tsp = 5 mL
- Tablespoon (tbsp): 1 tbsp = 15 mL
- Cup: 1 cup = 240 mL
- In addition to the metric system, nurses often encounter household measurements, particularly in pediatric dosing. Common units include:
- Converting Household Measurements to Metric:
- Understanding how to convert household measurements to metric units is crucial for accurate dosing:
- Example: Convert 2 tsp to mL:
- 2 tsp × 5 mL/tsp = 10 mL
- Example: Convert 2 tsp to mL:
- Understanding how to convert household measurements to metric units is crucial for accurate dosing:
- Patient Education:
- When providing medication instructions, nurses must clearly explain dosing in familiar terms to enhance patient understanding and adherence.
Performing Dosage Calculations
Calculating medication dosages involves various methods, and nurses must be proficient in these techniques to ensure accuracy and safety.
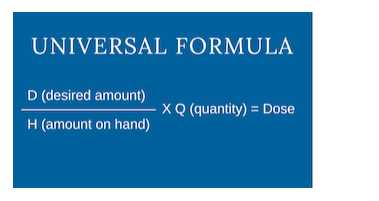
Methods for Dosage Calculations
- Ratio and Proportion:
- This method uses a simple equation to find the unknown quantity. The ratio of the prescribed dose to the available dose is set equal to the ratio of the unknown quantity to a known quantity.
- Formula:
- (Desired Dose / Available Dose) = (X / Quantity Available)
- Example:
- If a patient requires 500 mg of a medication that comes in 250 mg tablets, the calculation would be:
- (500 mg / 250 mg) = (X / 1 tablet)
- Cross-multiply: 500 mg = 250 mg × X
- Solve for X: X = 2 tablets
- If a patient requires 500 mg of a medication that comes in 250 mg tablets, the calculation would be:
- Dimensional Analysis:
- This method uses conversion factors to cancel out units and facilitate calculation. It is especially helpful for more complex conversions.
- Steps:
- Identify the desired unit.
- Write down the known quantities and their conversion factors.
- Arrange the conversion factors to cancel out units.
- Example:
- Calculate how many mL are needed if a patient requires 75 mg of a medication that is available in 25 mg/mL:
- Desired: 75 mg × (1 mL / 25 mg) = 3 mL
- Calculate how many mL are needed if a patient requires 75 mg of a medication that is available in 25 mg/mL:
- Algebraic Method:
- For more complex calculations, an algebraic approach can be beneficial. This involves setting up an equation to solve for the unknown.
- Example:
- If a patient needs 1.5 g of a medication that is supplied as a 0.5 g/5 mL solution, set up the equation:
- 1.5 g = (0.5 g/5 mL) × X mL
- Solve for X:
- 1.5 g / (0.5 g/5 mL) = X
- X = 15 mL
- If a patient needs 1.5 g of a medication that is supplied as a 0.5 g/5 mL solution, set up the equation:
- Calculating Doses for High-Alert Medications:
- High-alert medications (e.g., insulin, anticoagulants) require double-checking and verification to prevent errors.
- Implementing a systematic approach, including a second nurse’s verification, can enhance safety.
Practicing Calculations for Pediatric and Geriatric Populations
- Pediatric Dosing Considerations:
- Dosing for children often involves calculations based on weight or body surface area (BSA). Standard dosing guidelines provide safe ranges for medication administration.
- Weight-Based Dosing:
- Doses are commonly calculated in mg/kg.
- Example: If a child weighs 20 kg and the prescribed dose is 10 mg/kg:
- Total Dose = 20 kg × 10 mg/kg = 200 mg
- Body Surface Area (BSA) Dosing:
- BSA calculations can provide more accurate dosing, especially for chemotherapy and other high-risk medications. The most common formula for BSA is the Mosteller formula:
- BSA (m²) = √((height (cm) × weight (kg)) / 3600)
- Example: A child weighing 15 kg and 100 cm tall:
- BSA = √((100 × 15) / 3600) ≈ 0.1 m²
- BSA calculations can provide more accurate dosing, especially for chemotherapy and other high-risk medications. The most common formula for BSA is the Mosteller formula:
- Geriatric Dosing Considerations:
- Older adults often have altered pharmacokinetics, including decreased renal function and changes in body composition, which can impact drug metabolism and elimination.
- Creatinine Clearance:
- Calculating creatinine clearance (CrCl) is essential for adjusting dosages in elderly patients.
- The Cockcroft-Gault formula is commonly used:
- CrCl (mL/min) = ((140 – age) × weight (kg) × (0.85 if female)) / (72 × serum creatinine (mg/dL))
- Example: An 80-year-old female patient weighing 70 kg with a serum creatinine of 1.2 mg/dL:
- CrCl = ((140 – 80) × 70 × 0.85) / (72 × 1.2) = 36.45 mL/min
- Polypharmacy Considerations:
- Older adults often take multiple medications, increasing the risk of drug interactions. Regular medication reviews and assessments are critical to ensure safety.
- Patient and Family Education:
- Engaging patients and their families in discussions about dosing, potential side effects, and the importance of adherence to prescribed regimens is crucial in both pediatric and geriatric populations.
Ensuring Accuracy in Calculating Doses for High-Alert Medications
- High-Alert Medications:
- High-alert medications are those that carry a higher risk of causing significant harm if used in error. These include anticoagulants, insulin, opioids, and certain chemotherapeutic agents.
- Implementing standardized protocols, such as double-checking calculations and using computerized physician order entry (CPOE) systems, can mitigate risks.
- Verification Processes:
- Establishing a culture of safety within healthcare teams is essential. Implementing double-check systems where a second nurse verifies calculations before administration can reduce the likelihood of errors.
- Use of bar-code medication administration (BCMA) systems enhances verification by ensuring the correct medication, dose, and patient match.
- Error Reporting:
- Encouraging open reporting of medication errors fosters a culture of learning and improvement. Analyzing errors and near-misses helps identify systemic issues and improve processes.
- Continuous Education:
- Ongoing training and education regarding dosage calculations, high-alert medications, and the importance of accuracy are critical for all healthcare providers. Regular competency assessments can ensure that staff remain knowledgeable and confident in their skills.
Conclusion
Mastering dosage calculations is essential for nursing practice. Understanding units of measurement, applying various calculation methods, and considering the unique needs of pediatric and geriatric populations are fundamental for providing safe and effective medication administration. By fostering a culture of safety, encouraging verification processes, and promoting continuous education, nurses can minimize the risk of medication errors and enhance patient outcomes. This knowledge not only ensures compliance with clinical guidelines but also empowers nurses to take an active role in patient care and safety.
