Expected Actions/Outcomes
In the realm of pharmacological therapies, understanding the expected actions and outcomes of medications is essential for providing safe and effective care. As a practical nurse (PN), you are responsible for assessing, monitoring, educating, and reinforcing appropriate medication use for your clients. This chapter will guide you through the processes involved in identifying a client’s expected response to medication, using resources to check on pharmacological agents, applying knowledge of pathophysiology, monitoring medication use over time, and reinforcing client education. Additionally, we will explore the importance of evaluating client responses to medications, including adverse reactions, therapeutic effects, interactions, and critical laboratory values.
-
Identify Client Expected Response to Medication

A critical aspect of nursing practice is understanding the expected responses that a patient will have to a prescribed medication. The expected response varies based on the class of drug, the condition being treated, the individual’s unique physiological state, and other factors.
1.1 Factors Influencing Medication Response
- Pharmacokinetics: The movement of the drug within the body (absorption, distribution, metabolism, and excretion) directly impacts how a client will respond to medication. For example, a patient with liver disease may have impaired drug metabolism, leading to a higher risk of drug toxicity.
- Pharmacodynamics: The study of the biochemical and physiological effects of drugs and their mechanisms of action. For example, an antihypertensive medication should lower blood pressure in patients with hypertension.
- Patient-Specific Factors: Age, gender, genetics, comorbid conditions, renal and hepatic function, and weight all influence how a patient will respond to a medication. For instance, children or elderly individuals may metabolize drugs more slowly, requiring adjusted doses.
- Drug Interactions: Medications may interact with each other, influencing the therapeutic or adverse effects of one or both drugs. The expected response must be considered in light of any other medications the patient is taking.
1.2 Common Expected Responses by Medication Class
- Antihypertensives: Expected responses include a reduction in blood pressure, typically accompanied by a decrease in heart rate (depending on the medication class, such as beta-blockers).
- Antibiotics: The expected response is the reduction or eradication of the infection, as demonstrated by a decrease in symptoms such as fever, swelling, or discharge.
- Analgesics (Pain Relievers): For pain medications, the expected response would be a reduction in pain severity, as measured by pain scales (e.g., 1-10 scale), often accompanied by improved mobility and function.
- Antidiabetics (Insulin, Oral Hypoglycemics): Expected outcomes include the stabilization of blood glucose levels within a normal range, reducing the risk of hyperglycemia or hypoglycemia.
- Anticoagulants (e.g., Heparin, Warfarin): The expected response is the prevention of blood clot formation or the thinning of the blood to reduce the risk of conditions like deep vein thrombosis (DVT) or pulmonary embolism (PE).
-
Use Resources to Check on Purposes and Actions of Pharmacological Agents
In clinical practice, nurses must have access to reliable resources to ensure the correct administration of medications. Understanding the purpose and action of pharmacological agents is essential for ensuring patient safety and therapeutic efficacy.
2.1 Common Resources for Pharmacological Information
- Drug Reference Books: Resources such as Lexicomp, Davis’s Drug Guide for Nurses, and Drugs.com are widely used for providing information on drug indications, pharmacodynamics, dosages, side effects, and interactions.
- Pharmacy Resources: Pharmacists are valuable resources for providing guidance on drug actions, recommended doses, potential interactions, and contraindications.
- Online Databases: Websites like UpToDate and the National Institutes of Health (NIH) provide up-to-date and evidence-based information on medications.
- Institutional Protocols and Guidelines: Each healthcare facility often has its own set of drug administration protocols, which include specific doses, routes, and schedules for medications. Nurses should familiarize themselves with these resources to ensure proper medication administration.
2.2 Evaluating Drug Actions and Effects
When using these resources, it is important to focus on the following drug attributes:
- Indication: Why the drug is prescribed (e.g., treating hypertension, controlling diabetes).
- Mechanism of Action: How the drug works at the molecular or cellular level to exert its therapeutic effects (e.g., beta-blockers reduce heart rate by blocking beta-adrenergic receptors).
- Side Effects and Adverse Reactions: Common and rare side effects (e.g., nausea, dizziness, or a serious allergic reaction).
- Contraindications and Precautions: Situations or conditions where the drug should not be used (e.g., a contraindication for NSAIDs in a patient with a history of peptic ulcers).
2.3 Keeping Updated on New Medications
New medications and treatments are continually being developed. Nurses should remain updated on emerging pharmacological agents, especially those recently approved by the FDA, which may have novel mechanisms of action or new safety concerns.
- Apply Knowledge of Pathophysiology When Addressing Client Pharmacological Agents
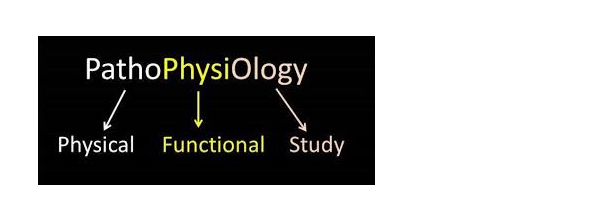
Understanding pathophysiology is vital when addressing pharmacological agents. Pathophysiology refers to the functional changes that occur in the body due to disease. By applying this knowledge, nurses can better understand how medications work to treat specific conditions.
3.1 Pathophysiology and Medication Mechanism of Action
- Hypertension: When treating hypertension with medications like ACE inhibitors or calcium channel blockers, nurses must understand the physiological changes that cause high blood pressure, such as vasoconstriction or fluid retention, to understand how the medication works to alleviate these conditions.
- Heart Failure: Medications like diuretics or ACE inhibitors help reduce fluid buildup and ease the heart’s workload. Understanding the pathophysiology of heart failure, such as poor ventricular contraction and fluid retention, allows nurses to anticipate how these medications help improve the client’s symptoms.
- Asthma: When administering bronchodilators, understanding the pathophysiology of asthma—such as airway constriction and inflammation—helps nurses understand why the drug will help open the airways and reduce respiratory distress.
3.2 Drug Use in Different Disease States
- Renal Failure: In patients with kidney disease, drugs that require renal excretion may need dose adjustments or be avoided due to the risk of toxicity. For example, medications like lithium are often avoided or dosed cautiously in patients with renal failure.
- Liver Disease: Similarly, liver disease affects drug metabolism. Hepatic impairment can lead to the accumulation of drugs in the body, requiring dose adjustments to prevent toxicity (e.g., warfarin, acetaminophen).
3.3 Applying Pharmacological Knowledge to Practice
In practice, nurses must apply their understanding of both the medication and the disease to anticipate potential effects and complications. For example, in patients with diabetes, administering insulin requires not only knowing the dose but also understanding the underlying pathophysiology of insulin resistance and glucose metabolism.
-
Monitor Client Use of Medications Over Time (e.g., Prescription, Over-the-Counter, Home Remedies)
Monitoring a client’s use of prescription, over-the-counter (OTC), and home remedies is an essential aspect of comprehensive medication management. As patients may use various forms of medication, it is vital for nurses to track their medication regimens and ensure they are being used correctly and safely.
4.1 Tracking Prescription Medications
- Documenting and Reviewing Medications: Nurses should verify the accuracy of prescribed medications and their dosages, monitoring for changes over time, such as dose adjustments or medication switches.
- Monitoring for Compliance: Ensuring that patients are following their prescribed regimen correctly, including taking medications at the right times and in the correct doses.
4.2 OTC and Home Remedies
- Common OTC Medications: These include pain relievers, cold and allergy medications, and antacids. Nurses must ask patients about OTC medications to ensure there are no adverse interactions with prescription medications.
- Herbal and Home Remedies: Many patients use herbal or alternative treatments. Nurses should be familiar with common herbs (e.g., garlic, ginseng) and their potential interactions with prescribed medications. For example, St. John’s Wort is known to interact with antidepressants.
4.3 Client Monitoring Over Time
Ongoing monitoring is crucial, as patients’ conditions or responses to medications may change over time. Adjustments to treatment plans should be made based on the patient’s evolving clinical condition and any adverse effects that arise.
-
Reinforce Education to Client Regarding Medications

Patient education is a cornerstone of safe and effective pharmacological therapy. Nurses must reinforce education to ensure clients understand how to take their medications correctly and safely.
5.1 Key Points of Medication Education
- Purpose of Medication: Explain why the medication is prescribed and how it works to treat the condition.
- Dosage and Timing: Ensure the patient understands the proper dosage, frequency, and method of administration (e.g., oral, injectable).
- Side Effects: Provide information on potential side effects and what to do if they occur.
- Adherence to Medication Regimen: Encourage patients to adhere to the prescribed schedule and not stop medications without consulting their healthcare provider.
5.2 Tailoring Education to Patient Needs
Patient education should be tailored to the individual’s understanding and needs, using clear language and culturally sensitive methods. For example, elderly patients may benefit from a larger print on medication labels, while pediatric patients might need more creative ways to understand their treatment.
-
Reinforce Client Teaching on Actions and Therapeutic Effects of Medications and Pharmacological Interactions
Reinforcing knowledge about medication actions, therapeutic effects, and pharmacological interactions is critical for clients’ safety.
6.1 Medication Actions and Therapeutic Effects
Educating the client about the intended therapeutic effects ensures they understand what they should expect from the medication. For instance, with pain medications, the patient should be aware that they should feel relief from pain, which will help them in their recovery process.
6.2 Pharmacological Interactions
Teach patients about potential interactions between medications. For instance, mixing certain antibiotics with alcohol can reduce their effectiveness, while taking multiple sedatives can lead to dangerous sedation. Reinforce the importance of consulting healthcare providers before adding new medications.
-
Evaluate Client Response to Medication
Evaluating a client’s response to medication is an ongoing process. It involves assessing therapeutic effects, side effects, interactions, and critical laboratory values.
7.1 Assessing Therapeutic Effects
The goal is to evaluate whether the medication has achieved the intended therapeutic effect. For example, after administering an antihypertensive, a nurse should assess whether the patient’s blood pressure has lowered to the desired level.
7.2 Adverse Reactions and Interactions
Monitoring for adverse reactions involves understanding the typical side effects of medications and recognizing any that are unexpected. For instance, allergic reactions, like rash or swelling, must be reported immediately.
7.3 Critical Laboratory Values
Certain medications require close monitoring of lab values to ensure safety. For example, potassium levels should be monitored when a patient is on a diuretic to avoid hypokalemia.
Conclusion
A comprehensive understanding of the expected actions and outcomes of medications is crucial in providing safe and effective care. Nurses must assess, monitor, and educate patients on the proper use of medications, reinforcing knowledge about therapeutic effects, side effects, and pharmacological interactions. By applying knowledge of pathophysiology and remaining vigilant in monitoring patients over time, nurses ensure optimal therapeutic outcomes and minimize risks associated with medication therapy.
