Provide care to a client with an ostomy (e.g., colostomy, ileostomy, urostomy)
-
Provide Care to a Client on a Ventilator
Overview:

A mechanical ventilator supports or replaces spontaneous breathing in patients with compromised respiratory function. Nursing care for ventilator patients includes monitoring ventilation, preventing complications, and ensuring optimal oxygenation.
Key Considerations:
- Indications for Ventilator Use: Acute respiratory distress, respiratory failure, postoperative recovery, drug overdose, or trauma.
- Types of Ventilators:
- Positive Pressure Ventilators: Commonly used in intensive care settings.
- Non-invasive Ventilators: Used for conditions like COPD exacerbations.
Nursing Responsibilities:
- Monitor Ventilator Settings: Check ventilator settings such as tidal volume, rate, and oxygen concentration (FiO2).
- Assess for Ventilator Complications: Common complications include ventilator-associated pneumonia (VAP), barotrauma, and ventilator-induced lung injury.
- Assess Patient’s Respiratory Status: Monitor oxygen saturation, respiratory rate, and end-tidal CO2 levels.
- Airway Management: Ensure the endotracheal tube or tracheostomy is securely positioned.
- Sedation and Analgesia: Administer prescribed sedatives and analgesics to prevent patient discomfort and agitation.
Patient Education:
- Family Education: Explain the purpose of mechanical ventilation, including how it will assist in the patient’s breathing while their condition stabilizes.
-
Provide Care for a Client Receiving Peritoneal Dialysis or Hemodialysis
Overview:
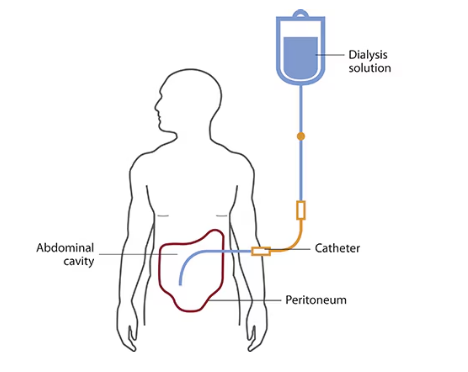
Dialysis is a procedure to remove waste products and excess fluid when the kidneys are unable to function. Peritoneal dialysis (PD) uses the peritoneum as a membrane, while hemodialysis (HD) uses an artificial kidney machine.
Nursing Responsibilities for Peritoneal Dialysis:
- Assess the Dialysis Site: Monitor the catheter insertion site for infection, inflammation, or leakage.
- Monitor Fluid Balance: Track inflow and outflow volumes of dialysis fluid.
- Check for Complications: Watch for signs of peritonitis (fever, abdominal pain, cloudy dialysate).
- Patient Education: Instruct the patient on how to perform home dialysis, manage sterile technique, and monitor for signs of infection.
Nursing Responsibilities for Hemodialysis:
- Prepare the Access Site: Inspect the arteriovenous (AV) fistula or graft for patency and signs of infection. Feel for a thrill and auscultate for a bruit.
- Monitor Vital Signs: Keep a close eye on BP, heart rate, and signs of fluid overload.
- Post-dialysis Care: Assess for complications like hypotension, arrhythmias, or electrolyte imbalances.
-
Provide Care to Correct Client Alterations in Body Systems
Overview:
Clients may experience alterations in their body systems, such as endocrine imbalances, fluid and electrolyte disturbances, or metabolic derangements. Nursing care includes identifying the cause of the alteration and providing appropriate interventions.
Nursing Responsibilities:
- Monitor Laboratory Values: Regularly check blood glucose, sodium, potassium, and calcium levels.
- Fluid and Electrolyte Balance: Administer IV fluids as prescribed and monitor urine output, signs of dehydration, or fluid overload.
- Endocrine Management: For clients with conditions like diabetes, manage blood sugar levels, insulin administration, and dietary modifications.
-
Provide Care to a Client Undergoing Peritoneal Dialysis
Overview:
Peritoneal dialysis (PD) uses the patient’s peritoneum as a semi-permeable membrane to filter waste and excess fluids from the blood. It can be performed at home or in a clinical setting.
Nursing Considerations:
- Access Site Care: Inspect the catheter insertion site daily for infection or leakage.
- Dialysate Monitoring: Monitor the inflow and outflow of dialysate for the correct amount and quality (clear dialysate is ideal).
- Complication Prevention: Watch for signs of peritonitis (e.g., fever, abdominal pain, cloudy dialysate).
- Post-dialysis Assessment: Check for abdominal distension, respiratory distress (due to fluid shifts), and monitor vital signs.
Patient Education:
- Sterile Technique: Teach patients the importance of maintaining aseptic technique when handling the dialysis catheter.
- Monitor for Complications: Educate patients about symptoms of infection and when to seek help.
-
Provide Care to a Client Experiencing Increased Intracranial Pressure (ICP)
Overview:
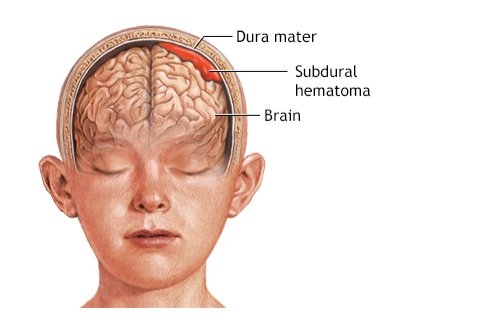
Increased intracranial pressure (ICP) can result from trauma, brain tumors, hemorrhage, or infections. Elevated ICP can lead to brain damage if not managed promptly.
Signs and Symptoms:
- Early Signs: Headache, nausea, vomiting, altered mental status.
- Late Signs: Pupillary changes, decreased LOC, bradycardia, irregular breathing patterns (Cheyne-Stokes), and hypertension.
Nursing Interventions:
- Positioning: Keep the head of the bed elevated to 30 degrees to enhance venous drainage.
- Monitor Vital Signs: Watch for changes in blood pressure (especially a widening pulse pressure) and heart rate.
- Medications: Administer prescribed medications like osmotic diuretics (e.g., mannitol) to reduce cerebral edema.
Patient Education:
- Positioning Education: Explain the importance of elevating the head to reduce ICP.
- Symptom Management: Teach the family signs of worsening ICP, such as changes in the patient’s responsiveness or worsening headaches.
-
Provide Care to a Client Who Has Experienced a Seizure
Overview:

Seizures result from abnormal electrical activity in the brain. Immediate care during and after a seizure focuses on ensuring safety, airway protection, and monitoring for complications.
Nursing Responsibilities:
- Ensure Safety: Protect the client from injury by moving harmful objects, cushioning the head, and loosening tight clothing.
- Airway Protection: Ensure that the airway is patent and clear after the seizure.
- Postictal Care: Assess the client for confusion, fatigue, or other post-seizure symptoms.
- Monitor for Complications: Watch for signs of status epilepticus or aspiration pneumonia.
Patient Education:
- Seizure Triggers: Teach the patient and family about possible seizure triggers (e.g., flashing lights, stress, sleep deprivation).
- Medications: Provide information on anticonvulsant medications, including side effects and the importance of compliance.
-
Provide Care for a Client Experiencing Complications of Pregnancy/Labor and/or Delivery
Overview:
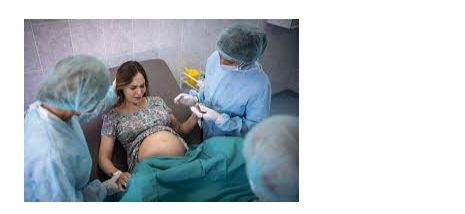
Pregnancy and childbirth can result in complications such as eclampsia, precipitous labor, or hemorrhage. These conditions require immediate nursing intervention.
Complications and Nursing Interventions:
- Eclampsia: A life-threatening condition characterized by hypertension and seizures. Administer magnesium sulfate to prevent seizures and monitor BP and reflexes.
- Precipitous Labor: Rapid labor may result in maternal or fetal trauma. Monitor maternal and fetal status and be prepared for an expedited delivery.
- Postpartum Hemorrhage: Monitor for signs of excessive bleeding, manage fundal massage, and administer uterotonics (e.g., oxytocin).
-
Perform Wound Care and/or Dressing Change
Overview:

Wound care is a critical aspect of patient recovery and involves proper cleaning, dressing, and monitoring for infection or complications.
Nursing Responsibilities:
- Assess the Wound: Observe for signs of infection, such as redness, swelling, or drainage.
- Wound Cleaning: Use sterile technique to clean the wound and change the dressing regularly to promote healing and prevent infection.
- Document Wound Characteristics: Record the size, appearance, and drainage of the wound for future reference.
-
Assist in the Care of a Client with a Pacing Device
Overview:
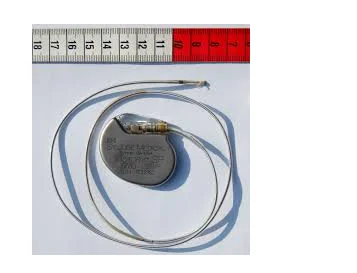
A pacemaker is a device implanted to regulate heart rhythm. Patients may require care following implantation or while troubleshooting issues related to the device.
Nursing Interventions:
- Monitor Pacemaker Function: Check for signs of malfunction, such as bradycardia or irregular heartbeats.
- Post-Implantation Care: Assess the insertion site for infection and hematoma.
- Patient Education: Instruct patients on lifestyle modifications and activity restrictions to avoid dislodging the pacemaker.
-
Remove Wound Sutures or Staples
Overview:
Removing sutures or staples is a common procedure performed after a wound has sufficiently healed to prevent further complications.
Nursing Procedure:
- Assess the Wound: Ensure the wound has healed appropriately with no signs of infection or dehiscence.
- Removal Technique: Use sterile equipment to carefully remove sutures or staples, ensuring the skin is not disturbed.
- Wound Dressing: Apply a sterile dressing after the procedure if necessary.
-
Assist with Client Wound Drainage Device Removal
Overview:
Wound drainage devices (e.g., Jackson-Pratt, Hemovac) are used to remove excess fluid from a wound to prevent infection.
Nursing Responsibilities:
- Assess Drainage: Check for signs of infection or abnormal drainage.
- Assist with Removal: Follow the healthcare provider’s instructions for the removal of drainage devices while minimizing patient discomfort.
-
Intervene to Improve Client Respiratory Status
Overview:
Nurses must assess and intervene to optimize the respiratory status of patients in need of breathing assistance.
Interventions:
- Breathing Treatments: Administer nebulizers or inhalers as prescribed.
- Suctioning: Suction secretions from the airway to ensure patency and oxygenation.
- Repositioning: Position the patient upright or on their side to facilitate optimal breathing.
-
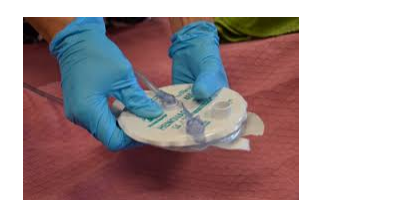
Reinforce Client Teaching on Ostomy Care
Overview:

Ostomy care involves the maintenance and management of a surgically created opening (stoma) to divert waste from the body.
Education:
- Hygiene: Teach clients how to clean and maintain the stoma and surrounding skin.
- Appliance Care: Instruct on the proper selection, application, and replacement of the ostomy bag.
- Watch for Complications: Educate clients on signs of infection, leakage, or blockage.
-
Reinforce Education to Client Regarding Care and Condition
Education Tips:
- Self-Care Techniques: Provide guidance on self-monitoring, including managing symptoms and using medical devices.
- Follow-Up Care: Ensure patients understand the importance of follow-up appointments for ongoing monitoring.
-
Notify Primary Healthcare Provider of a Change in Client Status
Overview:
Early detection and reporting of changes in a client’s status are vital to prevent complications.
Nursing Responsibilities:
- Monitor Vital Signs: Pay attention to sudden changes in blood pressure, heart rate, or respiratory status.
- Document and Report: Use clear communication to inform the healthcare provider of changes in clinical status or unexpected outcomes.
-
Document Client Response to Interventions
Overview:
Accurate documentation of patient responses to interventions is critical for effective care and future decision-making.
Documentation Tips:
- Document Observations: Record changes in vital signs, wound status, and symptoms.
- Evaluate Outcomes: Include responses to treatments, such as pain relief, wound healing, or respiratory improvement.
