Medication Administration
Medication Administration
Routes of Administration
Oral Medications

Understanding the Pharmacokinetics of Oral Medications
Pharmacokinetics involves the study of how drugs move through the body, encompassing four key processes: absorption, distribution, metabolism, and excretion.
Absorption: This is the process by which a drug enters the bloodstream from the site of administration. Oral medications typically undergo a series of stages before reaching systemic circulation:
- Dissolution: The medication must dissolve in the gastrointestinal (GI) tract, which is influenced by factors such as the formulation (tablet, capsule, liquid), presence of food, and pH of the gastric environment.
- Transport: Once dissolved, the drug molecules cross the intestinal mucosa. Lipid-soluble drugs are absorbed more readily than water-soluble drugs.
First-pass Effect: After absorption, the drug travels to the liver via the portal vein. The liver metabolizes a portion of the drug, reducing its bioavailability. The first-pass effect can significantly impact the dosage required for therapeutic effects:
- High First-pass Metabolism: Drugs with significant hepatic metabolism may require higher oral doses to achieve therapeutic levels.
- Low First-pass Metabolism: Medications that are minimally metabolized during their first pass through the liver may not require dose adjustments.
Techniques for Safe Oral Medication Administration
Administering oral medications requires adherence to best practices to ensure patient safety and medication effectiveness:
i. Crushing Pills: Some tablets can be crushed to facilitate administration, especially in patients who have difficulty swallowing (dysphagia). However:
- Check for Extended-Release Formulations: Extended-release (ER) or enteric-coated medications should never be crushed, as this can lead to rapid absorption and potential toxicity.
- Use of Liquid Forms: When possible, liquid formulations may be preferred for patients with swallowing difficulties. This ensures the full dose is delivered without compromising the drug’s efficacy.
ii. Administering Medications:
- Positioning: Ensure the patient is sitting upright or in a high-Fowler’s position to prevent aspiration.
- Using a Pill Organizer: For patients on multiple medications, a pill organizer can help manage complex regimens and ensure adherence.
- Water Intake: Encourage the patient to take medications with a full glass of water, unless contraindicated. This helps with swallowing and absorption.
Contraindications for Oral Medications
There are specific scenarios in which oral medication administration may be contraindicated:
- Dysphagia: Patients with difficulty swallowing may be at risk for aspiration, making oral administration unsafe.
- NPO Status: Patients who are NPO (nothing by mouth) for surgical procedures or medical conditions should not receive oral medications.
- Gastrointestinal Alterations: Conditions like nausea, vomiting, or significant diarrhea can impair absorption.
- Altered Consciousness: Patients who are unconscious or have impaired swallowing reflexes require alternative routes of administration.
Intramuscular (IM) Injections
Identifying Appropriate Sites for IM Injections
IM injections are commonly used for administering vaccines, hormones, and medications that require rapid absorption. Key sites include:
i. Deltoid Muscle:
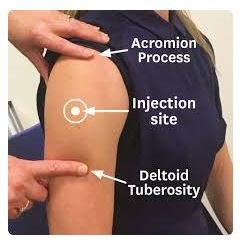
- Location: The deltoid muscle is located in the upper arm. It is easily accessible but has a limited volume capacity (generally up to 1 mL).
- Indications: Suitable for vaccines and some medications; the deltoid site is frequently used due to its convenience.
ii. Ventrogluteal Site:
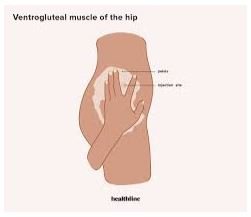
- Location: The ventrogluteal site is located on the lateral aspect of the hip. To locate, place the heel of your hand over the greater trochanter, point your thumb toward the groin, and your fingers toward the patient’s head.
- Indications: This site can accommodate larger volumes (up to 3 mL) and is less likely to cause injury to nerves and blood vessels, making it ideal for larger injections.
iii. Vastus Lateralis:

- Location: Located in the outer thigh, the vastus lateralis is a good option for children and infants.
- Indications: It is commonly used in pediatric populations and can hold up to 2 mL of medication.
Understanding the Volume Limits and Needle Sizes for IM Administration
Volume Limits:
- Deltoid: Up to 1 mL.
- Ventrogluteal: Up to 3 mL.
- Vastus Lateralis: Up to 2 mL (in adults).
Needle Sizes:
- Generally, 21-23 gauge needles are used for IM injections, depending on the viscosity of the medication.
- Length may vary: 1-1.5 inches for adults, and 0.5-1 inch for children, ensuring the needle penetrates the muscle adequately.
Techniques to Minimize Pain and Complications
Z-track Method: This technique minimizes irritation and leakage of the medication into the subcutaneous tissue:
Procedure:
- Displace the skin laterally before inserting the needle.
- Inject the medication and withdraw the needle while holding the skin in place.
- Release the skin to seal the medication in the muscle tissue.
Aspirate Before Injection: To ensure the needle is not in a blood vessel, some practitioners aspirate before injecting. However, recent guidelines have shifted away from this practice for most IM injections, particularly in the deltoid.
Intravenous (IV) Medications
Indications for IV Therapy
IV administration allows for rapid delivery of medications and fluids, suitable for:
- Rapid Effect: When immediate drug effects are required, such as in emergencies or severe dehydration.
- Fluid Resuscitation: For patients needing rapid volume replacement due to shock, hemorrhage, or dehydration.
- Medication Compatibility: Some medications are better absorbed when given IV, bypassing the first-pass metabolism.
Understanding Different Types of IV Fluids
IV fluids can be classified into two categories:
i. Crystalloids: These are solutions of minerals or other water-soluble molecules. They can be isotonic, hypotonic, or hypertonic:
- Isotonic Solutions: Maintain fluid balance (e.g., Normal Saline, Lactated Ringer’s).
- Hypotonic Solutions: Move water into cells (e.g., 0.45% NaCl).
- Hypertonic Solutions: Draw water out of cells (e.g., 3% NaCl).
ii. Colloids: These contain larger molecules that remain in the bloodstream, helping to expand blood volume (e.g., albumin, dextran). They are often used in patients with significant blood loss.
Recognizing Complications Specific to IV Administration
Common complications associated with IV administration include:
i. Phlebitis: Inflammation of the vein, often due to irritation from the IV catheter or medication. Signs include redness, swelling, and tenderness along the vein.
- Prevention: Use proper techniques for insertion and securement, and rotate sites regularly.
ii. Extravasation: Leakage of IV solution or medication into the surrounding tissue, potentially leading to tissue damage. Symptoms include swelling, pain, and blanching at the site.
- Management: Stop the infusion immediately, aspirate the area if possible, and follow protocol for specific medications.
iii. Infiltration: Unintentional leakage of IV fluid into the surrounding tissue, causing swelling and discomfort.
- Prevention: Monitor IV sites regularly and use appropriate catheter sizes.
Topical Medications
Techniques for Applying Topical Agents
Topical medications include creams, ointments, gels, and transdermal patches. Proper application techniques are crucial:
i. Ointments and Creams:
- Apply a thin layer to the affected area. Use gloves to prevent contaminating the medication and avoid skin contact.
- Rub the medication gently into the skin unless contraindicated. For larger areas, use a gentle patting motion to avoid further irritation.
ii. Transdermal Patches:
- Apply to clean, dry skin, free from hair, and rotate sites to prevent skin irritation.
- Remove the old patch before applying a new one to avoid overdose. Educate the patient on proper application and when to replace patches.
Assessing Skin Integrity Before Application
Before applying topical medications, assess the skin for:
- Integrity: Look for signs of breakdown, redness, or infection.
- Cleanliness: The area should be free from dirt or other products that may hinder absorption.
- Allergies: Ensure the patient has no known allergies to ingredients in the medication.
Patient Education on Proper Use and Potential Systemic Effects
Educating patients on the correct use of topical medications is essential:
- Application Instructions: Teach them how to apply the medication correctly and the importance of adhering to prescribed dosages and schedules.
- Potential Side Effects: Discuss possible local reactions (e.g., redness, itching) and systemic effects, particularly with transdermal patches, which may cause dizziness, headache, or nausea.
Medication Safety
The “Five Rights” of Medication Administration
The “Five Rights” framework is critical in ensuring safe medication administration:
i. Right Patient: Confirm the patient’s identity using two identifiers (e.g., name and date of birth) before administration.
- Identification Protocols: Utilize wristbands and verbal confirmation. Ensure that the patient can confirm their identity.
ii. Right Drug: Verify the medication against the prescription.
- Labeling: Check for correct labeling and expiration dates. Be wary of look-alike or sound-alike medications.
iii. Right Dose: Ensure the correct dose is calculated and verified.
- Calculation Methods: Utilize dosing calculators or consult with a pharmacy if uncertain. Double-check high-risk medications, such as anticoagulants.
iv. Right Route: Administer medications via the correct route as prescribed (oral, IM, IV, etc.).
- Understanding Formulations: Ensure the medication is suitable for the intended route, particularly for formulations that cannot be altered (e.g., enteric-coated).
v. Right Time: Administer medications at the prescribed time.
- Scheduling: Understand the importance of timing, particularly for medications with specific dosing intervals or those affected by food.
Error Prevention Strategies
Implementing Strategies to Prevent Medication Errors
Preventing medication errors is crucial for patient safety:
- Double-Checking: Encourage a culture of verification where nurses double-check calculations and high-risk medications.
- Using Technology: Implement bar-code medication administration (BCMA) systems, which use barcode scanning to confirm the right patient, drug, dose, route, and time.
- Standardizing Protocols: Establish clear protocols and checklists for medication administration, ensuring that all staff members follow the same procedures.
Reporting and Documenting Medication Errors
In the event of a medication error, it’s essential to follow facility protocols:
- Immediate Action: Assess the patient’s condition and provide necessary interventions.
- Reporting: Notify the supervising nurse and the physician immediately. Follow your facility’s reporting procedures.
- Documentation: Accurately document the incident in the patient’s medical record, including the medication involved, dose, route, time, and the patient’s response.
Conclusion
This comprehensive overview of Medication Administration in nursing practice emphasizes the importance of safe medication handling and the protocols necessary to ensure patient safety. By understanding the pharmacokinetics of medications, the appropriate administration routes, and the principles of medication safety, nurses can provide effective care that minimizes the risk of errors and optimizes therapeutic outcomes. Continuous education, adherence to best practices, and a commitment to patient safety are vital in nursing pharmacology and parenteral therapies.
