Prenatal Care and Fetal Development
Prenatal Care
Initial Prenatal Assessment
History-Taking:
i. Medical History:

- Chronic Conditions: Assess for chronic illnesses such as diabetes, hypertension, thyroid disorders, or autoimmune diseases. These conditions can significantly affect both maternal and fetal health. For instance, poorly controlled diabetes can lead to congenital anomalies or macrosomia (excessive fetal growth).
- Previous Pregnancies: Document any past pregnancies, including details on complications like preterm birth, gestational diabetes, preeclampsia, or cesarean sections. This information helps in identifying potential risks in the current pregnancy.
- Medications: Review current and past use of prescription medications, over-the-counter drugs, and herbal supplements. Some medications may be contraindicated or require dosage adjustments during pregnancy.
ii. Obstetric History:

- Menstrual History: Determine the length and regularity of menstrual cycles to estimate the gestational age of the pregnancy. This also includes the date of the last menstrual period (LMP), which is crucial for dating the pregnancy.
- Contraceptive Use: Inquire about past contraceptive use, including hormonal methods, intrauterine devices (IUDs), or barrier methods, as this can impact conception timing and pregnancy health.
iii. Family History:

- Genetic Conditions: Collect information on any genetic disorders or congenital conditions in the family. This may necessitate genetic counseling or screening.
- Health Conditions: Document family history of chronic illnesses such as cardiovascular disease, cancer, or mental health disorders, as these may influence maternal health and pregnancy outcomes.
Physical Examination:
i. General Health:
- Vital Signs: Measure blood pressure, heart rate, and respiratory rate to establish baseline values. Elevated blood pressure can indicate potential complications such as preeclampsia.
- Weight and Height: Assess weight to calculate body mass index (BMI). Significant deviations from normal BMI can affect pregnancy and delivery.
ii. Pelvic Examination:
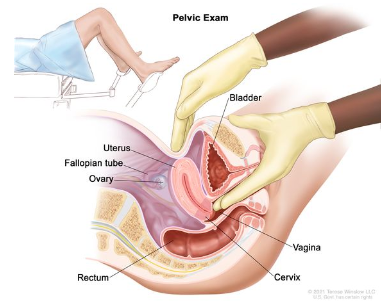
- Pelvic Anatomy: Examine the pelvic structures to assess the size, shape, and position of the pelvis, which can impact delivery.
- Cervical Assessment: Evaluate cervical length and consistency, which helps in predicting the risk of preterm labor.
Laboratory Tests:
i. Complete Blood Count (CBC):
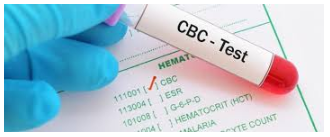
- Hemoglobin and Hematocrit: Measure to assess for anemia, which is common during pregnancy due to increased blood volume and iron demands.
- White Blood Cell Count: Elevated levels may indicate infection or inflammation.
ii. Blood Type and Rh Factor:
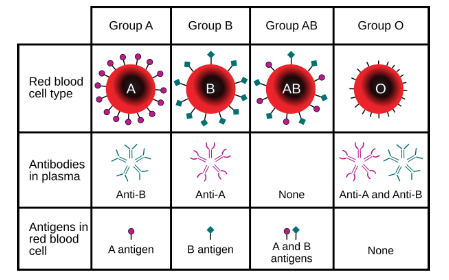
- Blood Type: Determine ABO blood group (A, B, AB, or O) to anticipate potential blood type incompatibilities.
- Rh Factor: Assess Rh status (positive or negative). If the mother is Rh-negative and the baby is Rh-positive, there is a risk of hemolytic disease of the newborn.
iii. Screening for STIs:
- Chlamydia and Gonorrhea: Screen for these common sexually transmitted infections, which can lead to complications such as preterm labor or neonatal infections.
- HIV Testing:

Offer testing to prevent mother-to-child transmission of HIV.
Routine Prenatal Visits
Frequency and Content of Visits:
i. First Trimester (Weeks 1-12):
- Frequency: Typically, visits are scheduled every 4-6 weeks.
- Content: Initial visits focus on confirming the pregnancy, establishing care, and performing baseline assessments.
ii. Second Trimester (Weeks 13-26):

- Frequency: Visits are usually scheduled every 4 weeks.
- Content: Routine checks include monitoring fetal development, screening for gestational diabetes, and addressing any new symptoms.
iii. Third Trimester (Weeks 27-40):

- Frequency: Visits increase to every 2 weeks until 36 weeks, then weekly until delivery.
- Content: Emphasis on assessing fetal well-being, preparing for labor and delivery, and discussing postpartum care.
Monitoring Vital Signs:
i. Blood Pressure:
Importance: Regular monitoring helps in early detection of hypertension or preeclampsia. Significant changes may necessitate further evaluation and intervention.
ii. Weight:
Tracking: Monitor weight gain to ensure it is within recommended ranges based on pre-pregnancy BMI. Excessive weight gain can indicate conditions like gestational diabetes.
Assessing Fetal Heart Tones and Growth:
i. Fetal Heart Tones:
- Doppler Device: Use a Doppler ultrasound device to listen to the fetal heartbeat, usually detectable by 10-12 weeks gestation. A normal fetal heart rate ranges from 120 to 160 beats per minute.
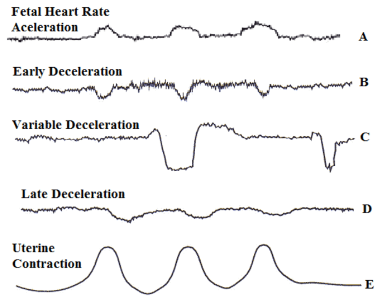
- Variability: Assess for normal variability and accelerations, which indicate fetal well-being.
ii. Fetal Growth:
- Fundal Height:
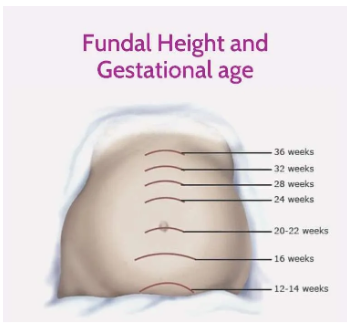
Measure the distance from the pubic symphysis to the top of the uterus (fundus) to estimate fetal growth and gestational age.
- Ultrasound: Use ultrasound to evaluate fetal growth, amniotic fluid levels, and placental position. Routine ultrasounds are typically performed around 20 weeks (anatomy scan) and as needed for any concerns.
Patient Education
Nutrition and Lifestyle Modifications:
i. Dietary Recommendations:
- Balanced Diet: Encourage a diet rich in fruits, vegetables, whole grains, lean proteins, and dairy to support fetal development and maternal health.
- Nutrient Needs: Emphasize the importance of folic acid, iron, calcium, and vitamin D. Folic acid is crucial for preventing neural tube defects, while iron supports increased blood volume and prevents anemia.
ii. Lifestyle Modifications:
-
- Avoiding Harmful Substances: Advise avoiding alcohol, tobacco, and recreational drugs, which can negatively impact fetal development.
- Environmental Toxins: Discuss reducing exposure to environmental toxins such as pesticides or certain chemicals.
Exercise and Prenatal Vitamins:
i. Exercise:
- Benefits: Encourage regular, moderate exercise, such as walking, swimming, or prenatal yoga, to improve circulation, reduce stress, and manage weight.
- Precautions: Advise on safety measures and modifications based on individual health conditions and fitness levels.
ii. Prenatal Vitamins:

- Importance: Recommend daily prenatal vitamins containing folic acid, iron, calcium, and other essential nutrients to support pregnancy and fetal development.
- Dosage: Advise on appropriate dosages and the importance of adherence to the prescribed regimen.
Warning Signs and When to Seek Help:
Emergency Symptoms:
- Severe Abdominal Pain: This could indicate conditions such as ectopic pregnancy, placental abruption, or preterm labor.
- Heavy Bleeding: Significant bleeding can be a sign of miscarriage, placenta previa, or other complications.
Other Concerns:
- Severe Headaches or Visual Changes: These symptoms may be related to preeclampsia or other serious conditions.
- Decreased Fetal Movement: A noticeable decrease in fetal movement after 28 weeks warrants immediate evaluation to assess fetal well-being.
Conclusion
In-depth prenatal care and fetal development encompass a comprehensive approach to maternal and fetal health. Initial assessments lay the foundation for personalized care, while routine visits monitor ongoing health and development. Patient education on nutrition, exercise, and warning signs equips expectant mothers with the knowledge to navigate pregnancy effectively. This holistic approach ensures that both mother and baby receive optimal care throughout the prenatal period.
